Employee benefits
New Jersey Pay Transparency Act Goes into Effect
As of June 1, 2025, New Jersey employers with 10 or more employees over 20 or more calendar weeks must comply with the New Jersey Pay and Benefit Transparency Act (“NJPBTA”). Covered employers include those doing business, employing individuals, or taking applications for employment within the state. What Does the Law Require?...
Read More
Medicare Creditable Coverage Disclosure Due to CMS by March 1, 2024
The Medicare Modernization Act (MMA) established annual notification requirements for employer-sponsored group health plans with prescription drug coverage. Per the MMA, employers sponsoring these plans are required to disclose annually the creditable status of the plan to The Centers for Medicare and Medicaid Services (CMS). This disclosure is due to...
Read More
7 Low-Cost Initiatives Employers Can Incorporate in Their D&I Programs Now
Countless studies show that employers who focus on diversity and inclusion policies and practices help increase employee engagement and boost overall happiness in the workplace, thus improving retention. Research shows that companies with diverse, inclusive teams generate 19% more revenue and perform 35% better than their industry average. While integrating...
Read More
Are You Leveraging Population Health Management Correctly to Mitigate Claims Risk?
While all health plans face the possibility of higher claims, properly managing your employee’s risk pool and population health can help mitigate claims risk and reduce costs in your plan. Population health management identifies, evaluates, and manages the risks facing an organization and its plan participants. While employers cannot prevent...
Read More
Four Steps to Create a Stable Renewal Environment
Large renewal rate increases frustrate employers and plan sponsors each year. They might experience significant, double-digit rate hikes one year; a smaller uptick the second; and another large increase the third year. Owners, CFOs, and HR executives would prefer stable, predictable trends so they can better budget for future costs....
Read More
How to Reset & Reflect After Benefits Renewal Season
The hectic benefits renewal season is finally winding down for many employers, with open enrollment meetings and all the logistical challenges and decisions behind us for 2021. We’re ready to relax and move on to new challenges during the new year. But wait a second: maybe we shouldn’t put renewal season...
Read More
Government Distribution of Free at-home COVID-19 tests
Starting January 19th, 2022, Americans will be able to order a test online at COVIDTests.gov. To ensure broad access, the program will limit the number of tests sent to each residential address to four tests. Tests will usually ship within 7-12 days of ordering. To help distribute the message to...
Read More
How to Reset and Reflect After Benefits Renewal Season
The hectic benefits renewal season is finally winding down for many employers, with open enrollment meetings and all the logistical challenges and decisions behind us for 2021. We’re ready to relax, enjoy the holiday season, and move on to new challenges during the new year. But wait a second: maybe we...
Read More
End of Year Employee Benefits Compliance Checklist
From ACA reporting to new federal regulations, employers are faced with several obligations as they close out the year and begin to plan for 2022. To help comply with your obligations, we have complied a list of important items that apply to employer-sponsored group health plans to either review and/or...
Read More
How We Resolved One Client’s Self-Funding Worries Through Proprietary Confidence Projection
Client Industry: Technology Number of Employees: 240 Service Provided: Statistical risk analysis and probability projections. Challenges Our client had considered transitioning from fully insured to self-funding for several years. Although we projected the change would bring considerable savings, they remained concerned by the risk that the model might not perform...
Read More
IRS Issues 2022 FSA and Commuter Limits
The IRS has announced the 2022 max contribution limits for FSA and Commuter accounts [Revenue Procedure 2021-45]. All FSA and Commuter plans (for the 2022 plan year) will be updated with the 2022 contribution limits. If you have any questions, please contact your account team or email us at icomply@ibpllc.com....
Read More
Innovative Saves Company From a $440,000 Renewal Increase with 45 Days Till Renewal
Challenges A construction company with 100 employees was facing a 29 percent renewal increase for its employee benefits package. The additional cost, which was over $440,000, was much more than the company could absorb. Passing the costs on to the employees through less coverage and higher deductibles seemed like the...
Read More
Employers COVID-19 Vaccine Resources & Kit
Sometimes it’s hard to keep up with all the latest recommendations and regulations. In an effort to ease the burden, we have compiled eight important resources that you can access when planning your COVID-19 vaccine practices. Access Here
Read More
Innovative Launches New Groundbreaking Benefit Performance Assessment
Innovative Launches New Groundbreaking Benefit Performance Assessment Innovative has launched our new groundbreaking, proprietary Benefit Performance Assessment. This complimentary assessment shows employers how they can cut waste, take control of healthcare costs, and provide better service solutions. All within an hour of your time and without impacting the coverage offered...
Read More
3 Reasons Every Employer Should Benchmark Their Health Plan
3 Reasons Every Employer Should Benchmark Their Health Plan As employers are competing for the race for talent and trying to bend the rising health care cost curve, benchmarking employee benefits is more important than ever. Here are three advantages to benchmarking health benefits: Bragging Rights: Employee benefits are a...
Read More
4 Ways to Leverage National Insurance Awareness Day to Increase Employee Awareness and Participation
June 28th is National Insurance Awareness Day! It was created as a day to review your insurance coverage and is also a great time to help your employees understand the benefits that are available to them. Focus today on empowering your employees to better understand, appreciate and participate in their...
Read More
Supreme Court Effectively Upholds ACA in Texas v. United States Ruling
Supreme Court Effectively Upholds ACA in Texas v. United States Ruling On June 17, 2021, the U.S. Supreme Court upheld the constitutionality of the Patient Protection and Affordable Care Act (ACA) by a 7-to-2 vote. The Court heard oral arguments in the case, California v. Texas, on November 10, 2020,...
Read More
4 Ways Digital Open Enrollment Guides Improve Employee Engagement
4 Ways Digital Open Enrollment Guides Improve Employee Engagement Every year open enrollment season allows employees to start, stop, or change their existing health insurance plans. Often, however, open enrollment can be a source of confusion, leaving employees with a lack of understanding and underutilizing their plan. Digital open enrollment...
Read More
BCBSA Antitrust Settlement Classes Eligible for Proceeds
BCBSA Antitrust Settlement Classes Eligible for Proceeds November 5, 2021 is the deadline for filing a claim in connection with the Blue Cross Blue Shield Association (BCBSA) $2.67 billion settlement reached in October 2020. The class action lawsuit was filed more than eight years ago by subscribers seeking injunctive and...
Read More
Why Employers Should Benchmark Their Health Plan Before Renewal
Why Employers Should Benchmark Their Health Plan Before Renewal Benchmarking your health plan during renewal ensures that the benefits being offered continue to be a right fit for the company and employees based on data-driven decisions. On the other hand, a poorly planned renewal done in the dark can cause...
Read More
IRS Issues 2022 HSA and HRA Limits
IRS Issues 2022 HSA and HRA Limits The IRS issued Revenue Procedure 2021-25 on May 10, 2021, to announce the 2022 inflation adjusted amounts for health savings accounts (HSAs) under Section 223 of the Internal Revenue Code (Code) and the maximum amount that may be made newly available for excepted...
Read More
5 Reasons Employers Should Carve Out Prescription Drug Benefits
5 Reasons Employers Should Carve Out Prescription Drug Benefits Prescription Drugs typically makes up 20% of an employer’s overall spend, and with the rise in specialty drugs, industry experts expect that number to encroach 50%. Employers have the ability to “carve-out” this coverage from their medical plan, resulting in significant...
Read More
Innovative Launches New Online Health Plan Benchmarking Tool
Innovative Launches New Online Health Plan Benchmarking Tool Benchmarking is more important than ever. Knowing how your health plan compare to your peers allows you to be competitive in recruiting and retaining the best employees, assist with making data-driven decisions during renewal planning, and see how your health plan costs...
Read More
Innovative Launches New Digital Employee Benefit Guide Technology
Innovative Launches New Digital Employee Benefit Guide Technology As technology continues to transform the workplace, HR professionals are seeking new and improved ways to deliver their health plan benefits, while gaining rich backend intelligence to improve the utilization of the plan. We have the solution! Innovative Benefit Planning is excited...
Read More
Innovative’s 2020 Consulting Highlights
Innovative’s 2020 Consulting Highlights 2020 was a challenging year for many, but here at Innovative, we were dedicated to delivering the best value and results for our clients. Not only were we successful in reducing costs for our clients, but we were able to provide them with a number of...
Read More
Is Level Funding a Good Fit for Your Employee Benefits Plan?
Is Level Funding a Good Fit for Your Employee Benefits Plan? Level funding is a great strategy for employers that are interested in self-funding, but like a plan that looks and feels like it is fully insured. Level funding acts just like a fully insured plan, except it provides the...
Read More
Final Rule on the Extension of Certain Timeframes For Employee Benefit Plans, Participants, and Beneficiaries Due to COVID-19
Final Rule on the Extension of Certain Timeframes For Employee Benefit Plans, Participants, and Beneficiaries Due to COVID-19 The DOL issued EBSA Disaster Relief Notice 2021-01 providing that the outbreak period relief noted below ends on the earlier of one year from the date an individual or plan was first...
Read More
Incorporating Wellness into Your Employee Benefits Strategy
Incorporating Wellness into Your Employee Benefits Strategy Wellness is a strategy that continues to gain in popularity as employers are looking for ways to help their employees become healthier, more engaged, and happier at work. Wellness is typically broken into three categories. The first category is educational wellness. With an...
Read More
Reference Based Pricing
Reference Based Pricing With healthcare costs skyrocketing at unsustainable levels, employers are considering nontraditional methods of funding their medical plans. One nontraditional method that employers are starting to consider is called reference based pricing, or RBR. This method has proven to reduce overall benefit spend 20 to 30%, when compared...
Read More
What is Bundled Pricing?
What is Bundled Pricing? Many employers are frustrated with a lack of financial and quality transparency in the healthcare marketplace. As such, many employers have considered offering a bundled pricing solution to their employees. Bundled pricing is a unique solution that provides employees the opportunity to shop for a procedure...
Read More
Understanding Captives and Consortiums
Understanding Captives and Consortiums As health insurance costs continue to rise, many small and mid-size employers have looked for ways to alternatively fund their plans and potentially save costs. Self-funding can be daunting and unmanageable for many small to mid-size employers, but there are many self-funding options to consider. Captives...
Read More
December Compliance Recap
December was a busy month in the employee benefits world. President Trump signed the Consolidated Appropriations Act, 2021, which includes the No Surprises Act and other group health plan provisions. The Centers for Disease Control Advisory Committee on Immunization Practices (ACIP) issued two interim recommendations for COVID-19 vaccines. The Department...
Read More
Mandatory Coverage of COVID-19 Vaccines under Group Health Plans
Mandatory Coverage of COVID-19 Vaccines Under Group Health Plans On December 11, 2020, the Food and Drug Administration (FDA) issued an Emergency Use Authorization for the Pfizer-BioNTech COVID-19 vaccine (Pfizer vaccine). The following day, December 12, 2020, the Centers for Disease Control Advisory Committee on Immunization Practices (ACIP) issued an...
Read More
November Compliance Recap
November Compliance Recap November was a relatively busy month in the employee benefits world. The U.S. Supreme Court (Supreme Court) heard oral arguments in the case of California v. Texas, which is the case challenging the constitutionality of the ACA. The Internal Revenue Service (IRS) released the updated Patient-Centered Outcomes...
Read More
Partially Self-Funded Plans with an HRA
Partially Self-Funded Plans with an HRA As health insurance costs continue to rise, more and more small and mid-size employers are looking for ways to take control of their healthcare costs. A health reimbursement account, or an HRA, is a way in which employers can step into self-funding and start...
Read More
Understanding Key Health Insurance Terms
Understanding Key Health Insurance Terms The language of health insurance can be confusing but understanding some key terms will help your employees comprehend the basics of your organization’s plan, allowing them to make smart decisions that will benefit their family. Rather than feeling confused, encourage them to review the following...
Read More
Final Rules on Coverage Transparency
Final Rules on Coverage Transparency On October 29, 2020, the Internal Revenue Service (IRS), Department of Labor (DOL), and the Department of Health and Human Services (HHS) (collectively, Departments), released final rules on coverage transparency, in order to provide health coverage recipients with an estimate of their potential cost-sharing liability...
Read More
6 Self-Funding Strategies to Suit Your Needs
6 Self-Funding Strategies Self-funding is nothing new as it has been a common form of health plan financing since 1974. Self-funding provides great flexibility with plan designs and provides freedom from most state laws. In fact, over 60% of US employees are covered under a self-insured medical plan. Under self-funded...
Read More
3 ACA Reporting Errors and The Pandemic’s Impact
3 ACA Reporting Errors and The Pandemic’s Impact As we approach the end of 2020, we must consider how the various enrollment fluctuations due to the COVID-19 Pandemic will impact the ACA Employer Mandate and the already tedious 1095/1094 ACA Reporting. The IRS recently granted a March 2nd deadline extension...
Read More
Have You Received an MLR Rebate Check? What To Do Next?
Have You Received an MLR Rebate Check? What To Do Next? The Affordable Care Act requires health insurance carriers to spend at least 80-85 percent of premium dollars on medical care and healthcare quality improvement. If the carrier does not meet this medical loss ratio (MLR) obligation, it must give...
Read More
August Compliance Recap
August 2020 Compliance Recap August was a relatively busy month in the employee benefits world. The Congressional Research Service (CRS) released an updated report on health savings accounts (HSAs) that summarizes the principal rules governing HSAs and changes made to HSAs as a result of the COVID-19 pandemic. The Department...
Read More
July Compliance Recap
July was a busy month in the employee benefits world. The U.S. Supreme Court (Supreme Court) upheld the religious exemption and moral exemption final rules to the Patient Protection and Affordable Care Act (ACA) contraceptive mandate. The Internal Revenue Service (IRS) released the indexed 2021 ACA affordability percentage. The President...
Read More
June Compliance Recap
June was a busy month in the employee benefits world. The Internal Revenue Service (IRS) released the updated patient-centered outcomes research institute (PCORI) fee amount and announced transition relief. The Department of Health and Human Services’ Office for Civil Rights (OCR) published a final rule regarding the Patient Protection and...
Read More
Judge Rules for HHS in Price Transparency Case
Judge Rules for HHS in Price Transparency Case A federal judge ruled against the American Hospital Association (AHA) on Tuesday in its lawsuit attempting to block an HHS rule pushing for price transparency. The judge ruled in favor of the department, which requires hospitals to reveal private, negotiated rates with insurers beginning...
Read More
HSA Limits Released for 2021
IRS issued the 2021 cost-of-living adjustments for Health Savings Accounts and High Deductible Health Plans. 2020 2021 Self-Only Contribution Limit $3,550 $3,600 Family Contribution Limit $7,100 $7,200 HDHP – self-only coverage Annual deductible not less than: Annual out-of-pocket expenses do not exceed: $1,400 $1,400...
Read More
Open Enrollment and Outcomes Based Health Screenings Options During COVID-19
Open Enrollment and Outcomes Based Health Screenings Options During COVID-19 Due to the COVID-19 outbreak, employers who were planning on offering on-site health screenings tied to payroll deductions are unfortunately being forced to consider other options. Thankfully, the screening vendors have been flexible with delaying screening dates. As an employer,...
Read More
Final Rule on the Extension of Certain Timeframes for Employee Benefit Plans Due to COVID-19
On March 13, 2020, President Trump issued the Proclamation on Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak and by separate letter made a determination, under Section 501(b) of the Robert T. Stafford Disaster Relief and Emergency Assistance Act, that a national emergency exists nationwide beginning March...
Read More
Paycheck Protection Program and Health Care Enhancement Act
Paycheck Protection Program and Health Care Enhancement Act In response to the spread of the 2019 novel coronavirus (COVID-19), President Trump signed the Paycheck Protection Program and Health Care Enhancement Act (PPPHCEA) into law on April 24, 2020. The PPPHCEA is phase 3.5 in Congress’ response to the COVID-19 pandemic...
Read More
Relaxed Life, Disability and Long-Term Care Insurance Underwriting
As a result of the COVID-19 National Emergency, insurance companies have adapted to help individuals easily secure protection and obtain insurance without a medical exam that requires a nurse to visit your home or office. This is a TEMPORARY change that will likely end when social distancing can stop. How...
Read More
March Compliance Recap
March was a busy month in the employee benefits world. The President signed the Families First Coronavirus Response Act (FFCRA) into law. The Department of Labor (DOL) issued a bulletin regarding enforcement of the FFCRA. The President also signed the Coronavirus Aid, Relief, and Economic Security Act (CARES Act) into...
Read More
Gov. Murphy Signs Executive Order Granting Grace Periods for Insurance Premium Payments
Gov. Murphy Signs Executive Order Granting Grace Periods for Insurance Premium Payments On April 9, 2020, New Jersey Governor Phil Murphy signed Executive Order No. 123, extending grace periods during which certain insurance companies, including health and dental insurers, life insurers, and property and casualty insurers, will not be able to...
Read More
COVID-19 Employer Considerations Regarding Employment Decisions and Plan Coverage Changes
Due to the recent national health crisis in our country, many employers are considering the best way to handle a temporary economic turndown to best position themselves for recovery once the pandemic ceases and businesses can begin to return to some sense of normalcy. In addition, many employers are also...
Read More
CARES Act: Impact on Employee Benefits
CARES Act: Impact on Employee Benefits On March 27, 2020, Congress passed, and the President signed, an unprecedented 2 trillion-dollar stimulus and relief package into law, named the Coronavirus Aid, Relief, and Economic Security Act or the CARES Act. This act provides direct stimulus relief to corporations and individuals. While...
Read More
Telemedicine Wait Times
In light of the recent COVID-19 (coronavirus) outbreak. The CDC recommends leveraging telemedicine for your unique medical needs to help limit the spread of the virus by eliminating the risk of exposure to the ER, urgent care, and primary care offices. They are recommending members schedule their virtual visits rather...
Read More
COVID-19: Carrier Enhancements
COVID-19: Carrier Enhancements March 17th, 2020 Due to the outbreak of COVID-19 in the United States, the CEO’s of major US health insurance companies met at the White House on March 10, 2020 and agreed to waive costs for certain services such as the COVID-19 test, telemedicine services and prescription...
Read More
Ways Employers Can Deal With Employee Student Loan Debt
Ways Employers Can Deal With Employee Student Loan Debt February 25th, 2020 Student debt has increased dramatically in recent years, creating a financial burden on employees’ ability to save for retirement. Many employers have begun implementing programs to help employees manage student loan debt. Millennials (and their families) are often...
Read More
December Compliance Recap
December was a busy month in the employee benefits world. The U.S. Court of Appeals for the Fifth Circuit held that the Patient Protection and Affordable Care Act’s (ACA’s) individual mandate is unconstitutional. The Internal Revenue Service (IRS) released final instructions and final 1094-B, 1095-B, 1094-C, and 1095-C forms for...
Read More
The ACA’s Cadillac, HIT and Medical Device Taxes Are Repealed; PCORI Fee Extended for 10 More Years
On December 20, 2019, the President signed a $1.4 trillion spending bill that will fund the federal government through September 30, 2020. The bill signed by the President specifically includes the repeal of three major taxes that fund the Affordable Care Act (ACA), including the “Cadillac” tax, the health insurance...
Read More
IRS Extends ACA Reporting Deadline for Furnishing Statements for 2019 from January 31 to March 2, 2020
In Notice 2019-63, the IRS extended the 2020 deadline for employers and insurers to furnish individual statements on 2019 health coverage and full-time employee status (Forms 1095-B and 1095-C) from January 31 to March 2. The notice also extends the good-faith penalty relief to 2019 for incorrect or incomplete reports due in 2020....
Read More
2020 IRS Contribution Limits Released
On Wednesday, the IRS announced new contribution limits for medical FSA, Commuter Benefit, and HSA plans for 2020. The FSA contribution will increase to $2,750, a $50 increase from current limits. The HSA contribution limit for individuals with a high deductible health plan (HDHP) will likewise be raised from $3,500...
Read More
September 2019 Compliance Recap
September was a busy month in the employee benefits world. The U.S. Senate confirmed Eugene Scalia as the new Secretary of the Department of Labor (DOL). The Internal Revenue Service (IRS) published proposed rules regarding affordability safe harbors and Section 105(h) nondiscrimination rules as applied to individual coverage health reimbursement...
Read More
Innovative Benefit Planning Named “Best of Biz 2019”
Innovative Benefit Planning has been named by South Jersey Biz, as one of their 2019 Best of Biz recipients. The Best of Biz award recognizes 102 of region’s most esteemed service providers and we are proud to say that Innovative has been selected for their “Employee Benefits” category. According to...
Read More
Additional Preventive Care Benefits Permitted for High Deductible Plans
In Executive Order 13877, issued June 2019, the Treasury Department and the IRS were directed to consider ways to expand the use and flexibility of HSA’s and HDHP’s. In response to the Executive Order, the Treasury Department issued guidance on July 17, 2019, that lists newly identified preventive care items...
Read More
Pennsylvania Medical Marijuana Updates
Effective July 20, 2019, Pennsylvania will recognize anxiety and Tourette Syndrome as serious medical conditions in the medical marijuana program. The Pennsylvania Department of Health stated that the decision came after a research-based recommendation by the state’s Medical Marijuana Advisory Board, followed by Health Secretary Rachel Levine ’s careful review of the...
Read More
HRA Final Rules
The Department of the Treasury (Treasury), Department of Labor (DOL), and Department of Health and Human Services (HHS) (collectively, the Departments) recently released their final rules regarding health reimbursement arrangements (HRAs) and other account-based group health plans. An HRA is a type of account-based group health plan funded solely by...
Read More
EEOC Component 2 Data Update
On July 2, 2019, following initial notifications to employers of the upcoming Component 2 filing deadline, the EEOC updated the Component 2 website to include both Additional Information https://eeoccomp2.norc.org/info.html and Frequently Asked Questions (FAQs) sections. https://eeoccomp2.norc.org/faq.html Under the Additional Information section, employers can find a sample form, an instruction booklet,...
Read More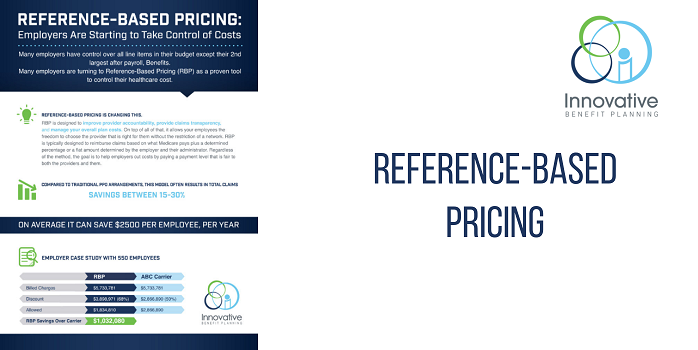
Reference-Based Pricing: Employers Are Starting to Take Control of Costs
You may have heard of Reference-Based Pricing as the healthcare strategy gains momentum to control healthcare costs. But what is it and how does it work? Click below to learn what Reference-Based Pricing is and the pros and cons to consider. Innovative’s unique Reference-Based Pricing 6 step process first makes...
Read More
NJ Now Has Greater Protections for Employees Who Are Cannabis Users
On July 2, 2019, New Jersey Governor Phil Murphy signed a bill into effect that overhauls the state’s existing medical cannabis program and law, the Compassionate Use of Medical Marijuana Act (CUMMA), and greatly expands patient access to medical marijuana. For employers who must address the issue of employees and...
Read More
HHS Proposes to Revise ACA Section 1557 Rule
On May 24, 2019, the Department of Health and Human Services’ Office for Civil Rights (OCR) released a proposed rule to revise its regulations under the Patient Protection and Affordable Care Act’s Section 1557. OCR also released a fact sheet and press release. The proposed rule would eliminate: Certain definitions,...
Read More
May 2019 Compliance Recap
May was a busy month in the employee benefits world. The Internal Revenue Service (IRS) released health savings account annual contribution limits and high deductible health plan minimum annual deductibles and annual out-of-pocket maximums for 2020. The Department of Labor (DOL) released questions and answers (Q&As) to clarify its enforcement...
Read More
EEOC Pay Data Collection
The Equal Employment Opportunity Commission (“EEOC”) announced that it will collect information from applicable employers on employee pay and hours-worked—known as Component 2 data—for 2017 and 2018 as part of the annual EEO-1 report and the data is due by September 30, 2019. The Department of Justice filed a Notice...
Read More
Compliance Alert: IRS Raises HSA/HDHP Limits for 2020
Compliance Alert: IRS Raises HSA/HDHP limits for 2020 The IRS has announced that effective January 1, 2020, an individual in a High Deductible Health Plan (“HDHP”) with self-only coverage has a new maximum allowable annual contribution into a Health Savings Account of $3,550 , increased from $3,500. The maximum annual...
Read More
April 2019 Compliance Recap
April was a busy month in the employee benefits world. The Centers for Medicare & Medicare Services (CMS) issued its parameters for the defined standard Medicare Part D prescription drug benefit for 2020. In the court case challenging the Patient Protection and Affordable Care Act’s constitutionality, the court will hear...
Read More
New NJ Commuter Law
Governor Murphy signed a new law on March 1, 2019, read here: Commuter Law, requiring certain employers to provide pre-tax commuter fringe benefits to employees. New Jersey employers with at least 20 employees in the state will need to begin offering those employees pre-tax transportation fringe benefits covering commuter highway vehicle...
Read More
March 2019 Compliance Recap
March was a busy month in the employee benefits world. The Department of Justice (DOJ) announced that it will not defend the Patient Protection and Affordable Care Act (ACA) in the court case challenging the ACA’s constitutionality. The Internal Revenue Service (IRS) updated two Q&As regarding ACA reporting for 2018....
Read More
Action-Based Wellness-How it Can Reduce Claims Cost 10-25%
See how Innovative helped one client save significant claims dollars over a three year period by implementing a “results-based” wellness program. During the three year period, Innovative was able to help our client: Obtain 96% of employees to participate in Biometric Screenings Implement a proactive outreach incentive program 60% of employees to improve or remain low...
Read More
Recent Updates in New Jersey Law
A lot has been happening in New Jersey since the new year began, and there have been a few critical updates for New Jersey employers and employees. New Jersey Minimum Wage On January 17, 2019, Governor Phil Murphy and legislative leaders agreed on legislation that will incrementally increase New Jersey’s...
Read More
Innovative Attends NAHU Capitol Conference
February 24-27th, Vice President Consulting Ryan Kastner, Director of Marketing Jamie Bratton and Vice President of HR & General Counsel, Deirdre Groenen, Esq. attended the 2019 NAHU Capitol Conference in Washington, DC. During their time in Washington, the trio attended three days of informative sessions that detailed changing legislation that...
Read More
December Compliance Recap
December was a relatively quiet month in the employee benefits world. A U.S. District Court issued an order declaring that the Patient Protection and Affordable Care Act (ACA) is unconstitutional. The Equal Employment Opportunity Commission (EEOC) issued two final rules to remove certain wellness program incentives. The Department of Labor...
Read More
10 FAQs Regarding The New Jersey Paid Sick Leave Act
1.) Earned sick leave may be used for: The treatment, care or diagnosis for employee or family member Employee or family member a victim of domestic or sexual violence (*has no 25 employees + or 1,000 hours worked requirement like the NJ Safe Act). Workplace or school/daycare closed by a public...
Read More
The IRS Increases the PCORI Fee
The Internal Revenue Service announced that the Patient-Centered Outcomes Research Institute (PCORI) fee will rise to $2.45 (from $2.39) per covered life in plan years that fall between October 1, 2018, and September 30, 2019. This increase will have an impact on 2019 plan year rates and is attributable to...
Read More
Tax Credit Check from Horizon
Attention Horizon customers! You may have received or will receive shortly, a check in the mail from Horizon regarding a tax credit refund check. Note, this is a legitimate check and you can use these funds however you see fit. Why are you receiving this check? In late 2017, the...
Read More
ACA Extensions Announced
Yesterday afternoon, the IRS released Notice 2018-94, which announced an extension of the 2019 deadline for insurers and employers to furnish forms 1095-B and 1095-C to individuals. These forms, originally due January 31, 2019 are now due March 4, 2019. Although the furnishing deadline has been extended, the IRS has...
Read More
Innovative Compliance- The New Jersey Equal Pay Act
As of July 1, 2018, the Diane B. Allen Equal Pay Act (“the Act”), which amends the New Jersey Law Against Discrimination (“LAD”), went into effect in New Jersey. The Act applies to all New Jersey public and private employers regardless of size, except federal employers. https://www.njleg.state.nj.us/2018/Bills/S0500/104_R2.PDF Pursuant to the...
Read More
New Tri-Agency Proposed Rule on Health Reimbursement Arrangements
The Department of the Treasury (Treasury), Department of Labor (DOL), and Department of Health and Human Services (HHS) (collectively, the Departments) released their proposed rule regarding health reimbursement arrangements (HRAs) and other account-based group health plans. The DOL also issued a news release and fact sheet on the proposed rule....
Read More
Important NJ Earned Sick Leave Update
In yesterday’s blog post, we discussed the New Jersey Earned Sick Leave Law, which went into effect this Monday, October 29th. For more on the specifics of the law. In addition to the employer obligations outlined in the previous post, all employers with employees working in New Jersey must post...
Read More
NJ Earned Sick Leave Law Goes into Effect
For New Jersey employers (or PA, NY or other employers who have employees who work in NJ), the NJ Earned Sick Leave Law went into effect Monday, October 29, 2018. Below is a link to a very comprehensive list of FAQs on the law, but here are some highlights: There...
Read More
Student Loan Considerations for Plan Sponsors-Part Two
As a follow up to our first article on student loan debt, its impact on employers and the recent IRS Private Letter Ruling (PLR) regarding student loan repayments, we’ve attached a summary of items to consider when contemplating this type of arrangement. As this ruling has just been released, we...
Read More
Innovative’s Executive Account Manager, Elizabeth Ferroni, attends Annual Employee Benefits Symposium
Our Executive Account Manager, Elizabeth Ferroni, just came back today from attending the Annual ISCEBS Employee Benefits Symposium in Boston, MA. Now in its 37th year, the symposium brings together thousands of benefit professionals to learn, discuss and hear from industry experts and leaders. Elizabeth is excited to be back...
Read More
Innovative Speaks at Leading Age NJ Annual Meeting & Expo
Last Wednesday, the Innovative team had the pleasure exhibiting and presenting at the Leading Age New Jersey Annual Meeting & Expo at Harrah’s Casino in Atlantic City, NJ. Innovative representatives, Dan Foley and Ryan Kastner, presented **Bucking the Trend: _Health Plan Cost Containment Strategies_** to an audience of aging services providers....
Read More
Compliance Alert! – NJ Gov. Phil Murphy Signs Two New Healthcare Acts into Law
This past week, New Jersey Governor, Phil Murphy, signed two bills into law that will impact New Jersey residents. Employers who offer benefits in New Jersey and surrounding states should be mindful of these changes as they will affect employees who reside and/or receive medical treatment in New Jersey. Out-of-network...
Read More
Horizon BCBSNJ Changes Coverage for Brand Name Oral-Combined Contraceptives
Starting June 15, 2018 , Horizon Blue Cross Blue Shield of New Jersey will be making changes to the way brand name oral-combined contraceptives are covered. Previously covered with a $0 copay, brand name oral-combined contraceptives will now be subject to co-payment or coinsurance that corresponds with the member’s pharmacy...
Read More
IRS Releases 2019 Calendar Year HSA Contribution Limits and HDHP Deductible Minimums and Out-of-Pocket Maximums
The IRS has released the maximum contribution limits for Health Savings Accounts (HSAs) and High Deductible Health Plan (HDHP) minimum deductibles and out-of-pocket maximums for the 2019 Calendar Year. For your convenience, we’ve provided a summary below. You can reference the official document here. Health Savings Account contribution limit for...
Read More
New Jersey Paid Sick Leave Act Signed into Law
New Jersey has now become the tenth state to enact a statewide mandatory paid-sick-leave law. The New Jersey Paid Sick Leave Act was signed into law on May 2nd by Gov. Phil Murphy and will go into effect on Oct. 29, 2018. Once effective, it will require New Jersey employers...
Read More
2018 Health Savings Account Contribution Limits Change Once Again
If you recall, after the passing of the tax reform bill, known formally as the Tax Cuts and Jobs Act, the IRS adjusted the amount for HSA family contributions from $6,900 to $6,850 due to a change in inflation calculations. After public outcry and consideration of the administrative and financial...
Read More
New Jersey Newborn Mandate Changes in 2018
In January 2018, the State of New Jersey updated the existing NJ Newborn Mandate that provides health coverage for all newborns from the moment of birth for the first 31 days to provide coverage from the moment of birth for the first 60 days. The newborn child of a subscriber...
Read More
March Compliance Recap
March was a quiet month in the employee benefits world. The Internal Revenue Service (IRS) released a bulletin that lowered the family contribution limit for health savings account (HSA) contributions. The U.S. Department of Labor (DOL) updated its model Premium Assistance Under Medicaid and the Children’s Health Insurance Program notice...
Read More
PrimeMail by Walgreens Gets a New Name
Effective 3/31/2018 PrimeMail by Walgreens Mail Service will operate under the name “Alliance RX Walgreens Prime“. Prime + Walgreens assures customers that only their name is changing. AllianceRX Walgreens Prime promises to stay consistent with their standards for communications, prescriptions, refills and service. Employers who have health plans with Horizon...
Read More
The Importance of Wellness in the Workplace
Workplace Wellness is an investment which works much like any other investment- You put in time and money in hopes of a more valuable outcome, which in this case is the health of your employees, their families and your bottom line. Engagement, motivation, strategy, and support are the keys to...
Read More
IRS RECALCULATES 2018 HSA & EMPLOYER ADOPTION ASSISTANCE PROGRAMS
Yesterday, the Internal Revenue Service (IRS) released a bulletin that includes a change impacting contributions to Health Savings Accounts (HSAs) and Employer Adoption Assistance Programs. The family HSA contribution for 2018 has been reduced from $6,900 to 6,850. This change is effective January 1, 2018. We advise plan participants to...
Read More
Focusing on FMLA
Human Resource professionals are often asked by their employees about taking a leave of absence. Sometimes, these leaves of absences are protected by the federal government. The Family and Medical Leave Act (FMLA) entitles eligible employees of covered employers to take unpaid, job-protected leave for certain medical and family reasons....
Read More
January Compliance Recap
January was a busy month in the employee benefits world. On January 24, 2018, the U.S. Senate confirmed Alex Azar as the new Secretary of the U.S. Department of Health and Human Services (HHS). The U.S. Department of Labor (DOL) proposed regulations regarding association health plans. HHS released the 2018...
Read More
Trump Signs Bill to Delay Cadillac and Health Insurance Taxes
On January 22, 2018, the U.S. Congress voted to pass a bill that would continue to fund the government through February 8, 2018. President Trump signed the bill today, January 23, 2018. In addition to continuing government funding, the bill also includes two legislative victories for employers: delaying the Cadillac...
Read More
IRS Announces Extension for Furnishing 1095-B & 1095-C Forms to Employees
Recently, the Internal Revenue Service announced an extension for employers to provide 1095-B or 1095-C Forms to their employees. The IRS announced a 30-day extension, extending the due date from January 31, 2018 to March 2, 2018. The IRS has not announced an extension for filings to the IRS. Therefore,...
Read More
IRS to Send ACA Penalty Letters
The Internal Revenue Service (IRS) has indicated that it plans to begin notifying employers by year end of their potential liability for failing to provide sufficient health coverage that is compliant with the Patient Protection and Affordable Care Act (ACA). The agency will begin notifying Applicable Large Employers (ALEs) of...
Read More
Innovative Partners with Morey’s Piers & Beachfront Water Parks
Innovative is excited to announce our new partnership with Morey’s Piers & Beachfront Water Parks. Morey’s Piers, located in Wildwood, New Jersey is an iconic seaside amusement park comprised of three amusement piers and two beachfront waterparks beloved by beachgoers far and wide. Innovative has been selected as the Benefit...
Read More
DOL Overtime Rule Defeated in Court, DOL to Appeal
As you may recall, the Department of Labor put forth overtime regulations that would have taken effect last December, enabling 4.2 million employees to be eligible for time and a half wages for every hour worked over the standard 40 hours per week. However, a number of business groups filed...
Read More
IRS Releases Maximum Contribution, Deferral and Compensation Limits for HSA, FSA, and 401(k) for 2018
The IRS has released the maximum contribution limits for Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs) for 2018. The IRS also released the maximum deferral and compensation limits for 401(k) accounts. Health Savings Accounts Single Coverage Maximum Contribution Limit: $3,450 ($50 increase from 2017) Family Coverage Maximum Contribution...
Read More
President Trump Ends ACA Cost Sharing Reductions
On the evening of October 12, 2017, President Trump announced that cost sharing reductions for low income Americans in relation to the Patient Protection and Affordable Care Act (ACA) would be stopped. The Department of Health and Human Services (HHS) has confirmed that payments will be stopped immediately. It is...
Read More
Compliance Alert!
Two tri-agency (Internal Revenue Service, Employee Benefits Security Administration, and Centers for Medicare and Medicaid Services) Interim Final Rules were released and became effective on October 6, 2017, and will be published on October 31, 2017, allowing a greater number of employers to opt out of providing contraception to employees...
Read More
Ryan Kastner Speaks at Pennsylvania State SHRM Conference
Earlier this morning, Innovative’s Employee Benefits Consultant, Ryan Kastner, had the pleasure of presenting at the Pennsylvania State SHRMconference in State College, PA. Ryan’s presentation, “Healthcare Trends in the Trumpcare Era” detailed the most recent national and regional employer health plan trends from the United Benefit Advisor’s Annual Health Plan...
Read MoreInnovative Employer Identity Monitoring and Restoration Services
Recently, Innovative had the pleasure of seeing Frank Abagnale speak at the UBA Conference in Chicago. You may recognize Frank’s name from the movie “Catch Me If You Can” where he was played by Leonardo DiCaprio. Frank became (in)famous for writing fake checks (among other things) as a teenager. Later...
Read More
Post-Equifax Cyber Breach: Retirement Plan Sponsor Considerations
Plan sponsors have a fiduciary obligation to safeguard and preserve the assets of their employee benefit plans. As the number of cyber hacks continues to increase, plan fiduciaries must take certain steps to protect plan assets. Measures include evaluating security measures currently implemented by your organization, understanding the plan’s service...
Read More
Post-Equifax Cyber Breach: Employer and Human Resource Considerations
Under EEOC regulations, employers can utilize credit checks when hiring employees, provided that the information is relevant to the position. For example, an individual who will be responsible for providing sound investment advice to clients, must prove to the company that their own credit is satisfactory. However, many vendors sell...
Read MoreRegarding the New York Paid Family Leave Law
NEW YORK PAID FAMILY LEAVE LAW Eligible employees will be able to take NYPFL to take care of a seriously ill family member, to bond with a newborn, adopted or foster child, or for military exigency, as defined by the federal FMLA rules. The New York Disability Benefits Law (NYDBL)...
Read More
ACA/BCRA Update
As you know, a few weeks ago Senate Republicans drafted a bill, the Better Care Reconciliation Act (“BCRA”), in an effort to repeal and replace the Patient Protection and Affordable Care Act (“ACA”). If you remember, Republicans currently hold a 52-member majority in the Senate, therefore Senate Republicans are left...
Read More
June Compliance Recap
June was an active month in the employee benefits world. The U.S. Senate released a draft of the Better Care Reconciliation Act of 2017 which would substitute the U.S. House Resolution 1628 that aimed to repeal and replace the Patient Protection and Affordable Care Act (ACA). The U.S. Supreme Court...
Read More
March Compliance Recap
In March, the employee benefits world watched as the House Speaker unveiled a proposal to replace parts of the Patient Protection and Affordable Care Act (ACA) with the American Health Care Act (AHCA). The AHCA bill was withdrawn from consideration by the full House on March 24 because it appeared...
Read More
February Compliance Recap
February had relatively little activity in the employee benefits world because a new Secretary of the Department of Health and Humans (HHS) was recently confirmed and HHS started its rulemaking under the new administration. On February 10, 2017, the U.S. Senate confirmed Rep. Tom Price as the new Secretary of...
Read More
Impact of Opt-Out Incentives on ACA Affordability Calculations
Quick Overview of Affordability Employers may find themselves subject to a penalty if an employee goes to the Marketplace/Exchange and obtains a premium credit, because the employer plan was not affordable or does not provide minimum value. An employee is not eligible for a premium tax credit for...
Read MoreNovember 2016- Compliance Recap
November was quite an active month for compliance related updates in the law with regard to employee benefits and human resources. The IRS delayed 6055 and 6056 reporting for 2017, the Overtime Rule was delayed, the government released annual benefit plan amounts for 2017, and the IRS released advanced copies...
Read MoreCompliance Alert! – DOL Appeals FLSA Overtime Rule Injunction
As we expected, last evening, the Department of Labor filed a notice of appeal in the Fifth U.S. Circuit Court of Appeals in New Orleans. The Department of Labor’s appeal indicates plans to challenge the injunction that put the changes to the federal overtime rule on hold by a Texas...
Read MorePhishing Email Alert
The Department of Health and Human Services has issued an alert regarding phishing attempts by a company or individual utilizing the HHS Departmental letterhead under the signature of OCR’s Director. The email appears to be an official government communication and targets employees of HIPAA covered entities and their business associates....
Read MoreFLSA Overtime Rule Blocked by Federal Judge
On Tuesday, November 22, 2016, a Texas federal judge blocked the Fair Labor Standards Act Overtime Rule by issuing a nationwide preliminary injunction. The regulation was scheduled to take effect on Dec. 1 and would have raised the salary limit for which workers could be exempt for overtime pay from...
Read MoreIRS Extends 1095 Deadline
The Internal Revenue Service has just announced an extension on the 2016 Form 1095-C , Employer Provided Health Insurance Offer and Coverage. Previously, the 1095-C was due to full time employees on January 31, 2017. Although the IRS had previously indicated not to expect an extension, an extension was granted...
Read More
The Trump Administration & Healthcare Reform
On January 20, 2017, Donald J. Trump will be sworn in as the next President of our nation. Next year, Republicans will have the majority in the House of Representatives (238 Republicans, 191 Democrats) and the majority in the Senate (51 Republicans, 47 Democrats). On November 14, 2016, House Republicans...
Read More
October 2016 Compliance Recap
October was a busy month for administrative rule-making in the employee benefits world. The Internal Revenue Service (IRS) released final instructions for Forms 1094-C and 1095-C, guidance on the taxability of health care sharing ministry employer contributions, and health care information reporting tips. The Department of Health and Human Services...
Read More
The Shift to Self-Funding
Year over year, more employers are making the switch from fully-insured health plans to self-funded arrangements. As of 2015, 63% of all covered employees are on completely or partially-funded employer health plans. Innovative Employee Benefits Consultant, Ryan Kastner, was quoted in MedCity News discussing the intricacies of self-funding. To read the...
Read More
Compliance Recap- September 2016
September was not a very active month for administrative rulemaking in the employee benefits world. The Internal Revenue Service (IRS), Department of Labor (DOL), and Pension Benefit Guaranty Corporation (PBGC) extended the public comment period for the proposed Form 5500 annual return/report revision. The IRS issued rules defining terms relating...
Read More
Innovative Attends United Benefit Advisor’s Fall Conference in Chicago
The Innovative team headed to Chicago this past weekend for the United Benefit Advisor’s Fall Conference September 18th-20th. “UBA is the nation’s leading organization of independent benefit advisors who are bound by a code of conduct to actively cultivate, validate and share wisdom with busy benefit decision makers nationwide who want...
Read More
How Corporate Wellness Programs Benefit You and Your Organization
Has your organization adopted a structured wellness program? Many employers are resistant to kickoff corporate wellness programs due to lack of knowledge and fear of high start up costs and increasing the workload on their busy Human Resources department. Read more in our Wellness Program Whitepaper about how you can...
Read More
August Compliance Recap
August remained relatively quiet in the employee benefits world, with only new draft versions of the instructions for Forms 1095-C, 1095-C, 1094-B and 1095-B. The new draft versions of the specific forms were released in July. The IRS also released the annual contribution limits for health savings accounts (HSAs) and...
Read More
August Compliance Recap
August was quiet month in the employee benefits world. The Internal Revenue Service (IRS) released its 2018 affordability rate, four information letters regarding the Patient Protection and Affordable Care Act (ACA), and its draft Forms 1094 and 1095. The U.S. Department of Labor (DOL) increased the McNamara-O’Hara Service Contract Act...
Read More
The Top 5 Things to Look for in an ACA Reporting Consultant
Innovative Benefit Planning’s consultants are widely considered the Affordable Care Act experts in the Greater Philadelphia and New Jersey areas. While many employers struggled with the ACA reporting for 2015 with little support, Innovative clients slept easy with employee communications, in-depth consultations, pre-form data audits, and error resolution support. Innovative...
Read More
HRAs, HSAs, and Health FSAs – What’s the Difference?
Health reimbursement arrangements (HRAs), health savings accounts (HSAs) and health care flexible spending accounts (HFSAs) are generally referred to as account-based plans. That is because each participant has their own account, at least for bookkeeping purposes. Under the tax rules, amounts may be contributed to these accounts (with certain restrictions)...
Read More
Employment Eligibility: How to Handle Questions about Worker Identity
Reports submitted to the U.S. government that include both names and Social Security numbers (SSNs), such as 1095 and W-2 forms, are filtered through U.S. Immigration and Customs Enforcement (ICE), a division of the Department of Homeland Security (DHS). In some cases, employers will receive a No-Match Letter or an...
Read More
Compliance Recap- July 2016
During the month of July numerous new regulations were issued or proposed by federal agencies, and existing forms and processes were updated. In particular, penalties for various ERISA violations were increased, a major overhaul to Form 5500 filings was proposed, and draft 1095-C and 1094-C forms were released. Proposed regulations...
Read More
Salary Considerations under the New DOL Standards
On December 1, 2016, the Department of Labor (DOL) will implement changes raising the minimum compensation for exempt employees to $47,476 annually. While salary is just half of a two-part equation that includes a duties test of essential job functions, scrutiny is under way to analyze compensation and find solutions...
Read More
June 2016 Compliance Recap
June was another quiet month for federal agencies in relation to employee benefits. A tri-agency proposed rule regarding expatriate health plans, excepted benefits, and essential health benefits was released. UBA Updates UBA’s Human Resources department released a checklist and advisor on new OSHA requirements: OSHA Reporting Changes: Employer Checklist OSHA’s...
Read More
Interim Final Rule Updating the Penalties for Certain ERISA Violations
In the beginning of July, the Department of Labor (DOL) issued an interim final rule, effective August 1, 2016, adjusting the amounts of civil penalties as required by the Federal Civil Penalties Inflation Adjustment Act Improvements Act of 2015. In order to improve the effectiveness of civil monetary penalties, maintain their deterrent...
Read More
Proposed Rule Offers Guidance on Expatriate Health Plans, Excepted Benefits and Essential Health Benefits
In a tri-agency proposed rule, the Department of Labor (DOL), Department of Health and Human Services (HHS), and Department of Treasury (Treasury) have published guidance discussing expatriate health plans (expat plans), excepted benefits, and essential health benefits (EHBs). Expatriate Health Plans The proposed rule would allow expatriate health plans, employers...
Read More
1095/1094 Reporting Accepted…with Errors?
Ryan Kastner – Employee Benefits Consultant Mid and large size employers have begun to breathe a sigh of relief knowing the first year of 1095/1094 Reporting is almost behind us. Unfortunately, 70% of employers are unable to fully relax as many are receiving notices of “filing discrepancies” within their 1095...
Read More
OSHA Issues a Final Rule on Electronic Tracking of Workplace Injuries & Illnesses
Is your organization tracking workplace illnesses and injuries in accordance with new laws? Beginning in 2017, certain employers with as few as 20 employees at a single site will be required to electronically file information about employee injuries and accidents that occurred in the prior year. This means that, for many...
Read More
Nondiscrimination Regulations Relating to Sex, Gender, Age, and More Finalized
On May 13, 2016, the Department of Health and Human Services (HHS) issued a final rule implementing Section 1557 of the Patient Protection and Affordable Care Act (ACA), which will take effect on July 18, 2016. If entities need to make changes to health insurance or group health plan benefit...
Read More
Seven Common Mistakes That Could Trigger a DOL Audit
Here are some great tips on how to avoid a DOL audit from the UBA Blog: Not many things incite more fear than receiving a notice that you’re about to have an audit, especially from the Department of Labor (DOL). The DOL is a cabinet-level department of the U.S. federal...
Read More
Compliance Recap – March 2016
The government was busy during the month of March, issuing the massive Benefit Payment and Parameters rule in addition to numerous other updates. The IRS has added filing errors relating to Form 5500 to its project list, and multiple federal agencies confirmed that the just-announced templates relating to the...
Read More
IRS Reporting Tip #2 – Form 1095-C, Line 14, Code 1A versus 1E, and When To Use 1I
Under the Patient Protection and Affordable Care Act (ACA), individuals are required to have health insurance, while applicable large employers (ALEs) are required to offer health benefits to their full-time employees. In order for the Internal Revenue Service (IRS) to verify that (1) individuals have the required minimum essential coverage,...
Read More
IRS Reporting Tip #1 – Form 1094-C, Line 22
Under the Patient Protection and Affordable Care Act (ACA), individuals are required to have health insurance while applicable large employers (ALEs) are required to offer health benefits to their full-time employees. In order for the Internal Revenue Service (IRS) to verify that (1) individuals have the required minimum essential coverage,...
Read MoreBenefit and Payment Parameters Rule and HIP FAQ
The 2017 Benefit and Payment Parameters (BPP) rule, an annual rule that sets policies relating to the Patient Protection and Affordable Care Act (ACA), has been released by the Centers for Medicare and Medicaid Services (CMS). The 2017 rule contains numerous updates, including the annual open enrollment periods for the...
Read More
Proposed Summary of Benefits and Coverage Template and Updates
A Summary of Benefits and Coverage (SBC) is four-page (double-sided) communication required by the federal government. It must contain specific information, in a specific order and with a minimum size type, about a group health benefit’s coverage and limitations. In February 2016, the Department of Labor (DOL) issued proposed revisions...
Read More
Compliance Recap- January 2016
January was a very quiet month for compliance, on the heels of the multitude of delays that came at the end of December 2015. The IRS updated its FAQs related to 6055 and 6056 reporting under the Affordable Care Act (ACA). UBA Guides and Compliance Documents UBA updated the popular...
Read More
IRS Updates FAQs Related to 6055/6056 Reporting
The long-standing IRS FAQs related to reporting under sections 6055 and 6056 on requirements provided by the Patient Protection and Affordable Care Act (ACA) have been updated in January 2016 to reflect new information. Final instructions for both the 1094-B and 1095-B and the 1094-C and 1095-C were released in...
Read More
Compliance Recap – December 2015
2015 went out with a bang, as federal agencies and the White House issued a number of major delays relating to employee benefits. Most significantly, IRS reporting for the Patient Protection and Affordable Care Act’s play or pay requirement has been delayed, for both forms being sent to employees and...
Read More
IRS Final Rule on Minimum Value
In December 2015, the Internal Revenue Service (IRS) issued a final rule that clarifies various topics relating to the Patient Protection and Affordable Care Act (ACA) and premium tax credit eligibility provisions. The rule finalizes regulations that were proposed years earlier. Child Income The final rule clarified language relating to...
Read More
IRS Provides Major Delay in 6055 and 6056 Reporting
Under the Patient Protection and Affordable Care Act (ACA), individuals are required to have health insurance, while applicable large employers (ALEs) are required to offer health benefits to their full-time employees. In order for the Internal Revenue Service (IRS) to verify that (1) individuals have the required minimum essential coverage,...
Read More
COBRA and the Affordable Care Act
The Consolidated Omnibus Budget Reconciliation Act COBRA requires employers to offer covered employees who lose their health benefits due to a qualifying event to continue group health benefits for a limited time at the employee’s own cost. COBRA provisions are found in the Employee Retirement Income Security Act (ERISA), the...
Read More
Omnibus Bill Signed Into Law; Delays Cadillac Tax
President Obama has signed the omnibus legislation that includes the Consolidated Appropriations Act for 2016 and a tax extenders package. The agreement will keep the federal government running through September 2016. Within the legislation is language that significantly impacts provisions of the Patient Protection and Affordable Care Act (ACA), largely...
Read More
IRS Notice 2015-87: HRAs, Affordability, and More
On December 16, 2015, the Internal Revenue Service (IRS) and other federal agencies released IRS Notice 2015-87, which is a “potpourri” update that covers many different topics relating to the Patient Protection and Affordable Care Act (ACA), including some relating to market reforms. The Notice generally covers health reimbursement arrangements...
Read More
Proposed Benefit Payment and Parameters Rule Released
Federal agencies have released the proposed rule for the 2017 Benefit Payment and Parameters. Among other items, it provides updates and annual provisions relating to: Risk adjustments, reinsurance, and risk corridors programs Cost-sharing parameters and cost-sharing reductions User fees for Federally-Facilitated Exchanges (FFEs) The standards for open enrollment for the...
Read More
Agencies Issue Final Rule on Grandfathered Health Plans and Other Initiatives
On November 13, 2015, federal agencies issued a final rule that essentially combined a variety of interim final rules and non-regulatory guidance on a variety of Patient Protection and Affordable Care Act (ACA) initiatives such as grandfathered health plans, preexisting condition exclusions, internal and external appeals, rescissions of coverage, lifetime...
Read MoreEEOC Issues Proposed Rule Relating to Genetic Information and Wellness Programs
On October 30, 2015, the Equal Employment Opportunity Commission (EEOC) issued a Proposed rule to amend the regulations implementing Title II of the Genetic Information Nondiscrimination Act (GINA) as they relate to employer wellness programs that are part of group health plans. The Proposed rule would allow employers to offer...
Read MoreIRS Notice on Minimum Essential Coverage Reporting
Minimum essential coverage or “MEC” is the type of coverage that an individual must have under the Patient Protection and Affordable Care Act (ACA). Employers that are subject to the ACA’s shared responsibility provisions (often called play or pay) must offer MEC coverage that is affordable and provides minimum value....
Read MorePerfect Attendance! – How to Handle Leaves of Absence under the ACA
The Patient Protection and Affordable Care Act (ACA) requires applicable large employers (ALEs) to offer full-time employees health coverage, or pay one of two employer shared responsibility penalties. An ALE is an employer with 50 or more full-time or full-time equivalent employees (for 2015, this threshold is 100). A full-time...
Read MoreTemporary Safe Harbor for Online Posting of SBCs
A Summary of Benefits and Coverage (SBC) is four-page (double-sided) communication required by the federal government under the Patient Protection and Affordable Care Act (ACA). It must contain specific information, in a specific order and with a minimum size type, about a group health benefit’s coverage and limitations. An SBC...
Read MoreHHS Proposes First of Anticipated Nondiscrimination Regulations
The Department of Health and Human Services (HHS) has issued the first of the anticipated nondiscrimination rules, which sets forth proposed regulations to implement Section 1557 of the Patient Protection and Affordable Care Act (ACA). Section 1557 provides that individuals shall not be excluded from participation, denied the benefits of,...
Read MoreAffordable Care Act Information Returns
Under the Patient Protection and Affordable Care Act (ACA), individuals are required to have health insurance while applicable large employers (ALEs) are required to offer health benefits to their full-time employees. In order for the Internal Revenue Service (IRS) to verify that (1) individuals have the required minimum essential coverage,...
Read More6055 Reporting, HRAs, and “Supplemental Coverage”
The Affordable Care Act (ACA) implemented section 6055 of the Internal Revenue Code, which requires IRS reporting from any entity that provides “minimum essential coverage” (MEC) to individuals. Employers who are applicable large employers (ALEs) have related reporting obligations under section 6056. Beginning in 2013, during the proposed rulemaking stage,...
Read MoreIRS Releases Draft 2015 Instructions for 6055/6056 Reporting
Under the Patient Protection and Affordable Care Act (ACA), individuals are required to have health insurance while applicable large employers (ALEs) are required to offer health benefits to their full-time employees. In order for the Internal Revenue Service (IRS) to verify that (1) individuals have the required minimum essential coverage,...
Read MoreVeterans with TRICARE; VA Coverage Won’t Count Toward Applicable Large Employer Status
The Surface Transportation and Veterans Health Care Choice Improvement Act (STVHCC) of 2015 was signed into law by President Obama on July 31, 2015. The Act, also known as H.R. 3236, is focused on surface transportation programs but affects rules regarding how to count employees under the Patient Protection and...
Read MoreIRS Issues Second Notice to Assist in Developing Cadillac Tax Regulations
The IRS has issued its second notice regarding the upcoming implementation of the Patient Protection and Affordable Care Act’s (ACA) excise tax on high cost employer-sponsored health coverage, also known as the “Cadillac tax.” Beginning in 2018, plans that provide coverage that exceeds a threshold will owe the tax. The...
Read MoreDOL Issues Guidance on Classification of Independent Contractors
The Department of Labor (DOL) has issued an “Administrator’s Interpretation” to assist employers in determining if a worker is an employee or an independent contractor. The DOL has determined that many employers are incorrectly classifying employees as independent contractors, which can harm the worker and open the employer up...
Read MorePreventive Services Final Rules
Federal agencies released final regulations on the preventive services mandate of the Patient Protection and Affordable Care Act (ACA) that requires non-grandfathered group health plans to provide coverage without cost-sharing for specific preventive services, which for women include contraceptive services. After pushback from religious employers, interim final regulations, objections from certain...
Read MoreMid-Size Employers: Transition Relief and Community Rating
The employer shared responsibility (i.e., “play or pay”) requirements went into effect in 2015 for large employers only (those with 100 or more full-time or full-time-equivalent employees). Even though they generally will not be liable for penalties until 2016, mid-size employers (employers with 50 to 99 full-time or full-time-equivalent employees)...
Read MoreTrade Bill Increases ACA Reporting Penalties;
Most employers are familiar with the penalties assessed to applicable large employers that fail to offer minimum essential coverage that is minimum value and affordable. In addition to being required to offer coverage, employers (all applicable large employers, and all employers with self-funded plans regardless of size) are required to...
Read MoreU.S. Supreme Court Finds Same Sex Marriage Is Protected by the 14th Amendment
The Supreme Court ruled in Obergefell v Hodges, that the 14th Amendment requires a state to license a marriage between two people of the same sex, and to recognize a marriage between two people of the same sex when their marriage was lawfully licensed and performed out of state. The...
Read MoreMid-Size Employers: Transition Relief and Community Rating
The employer shared responsibility (i.e., “play or pay”) requirements went into effect in 2015 for large employers only (those with 100 or more full-time or full-time-equivalent employees). Even though they generally will not be liable for penalties until 2016, mid-size employers (employers with 50 to 99 full-time or full-time-equivalent employees)...
Read More2015 Cost-of-Living Adjustments
Many employee benefit limits are automatically adjusted each year for inflation (this is often referred to as an “indexed” limit). The Internal Revenue Service and the Social Security Administration have released a number of indexed figures for 2015. Limits of particular interest to employers include the following. For health and...
Read MoreTransitional Reinsurance Fee Filing Date Extended to December 5
The Centers for Medicare and Medicaid Services (CMS) has extended the deadline for group health plans to complete their 2014 transitional reinsurance fee (TRF) submission. The announcement, which was released late on November 14, 2014, states that the filing is now due by 11:59 p.m. on Friday December 5, 2014....
Read More2015 Cost-of-Living Adjustments
The IRS has issued the cost-of-living adjusted figures for qualified plans and for several fringe benefits for 2015. Of particular interest to many employers are: • An increase in the maximum employee contribution to a health flexible spending account (HFSA) to $2,550 • An increase in the 401(k) and 403(b)...
Read MoreRequirement to Obtain a Health Plan Identifier (HPID) Delayed
On Friday October 31, 2014 the Department of Health and Human Services (HHS) quietly updated its Health Plan Identifier information page to delay the requirement that insurance carriers and self-funded health plans obtain a health plan identifier (HPID). The delay is in effect until further notice. Plans that have already...
Read MoreHighlights of Wellness Program Requirements
The wellness program rules provide an exception to the general rule that employers may not take a person’s health status into account with respect to eligibility, benefits, or premiums under a group health plan. Wellness programs, therefore, are allowed if they are designed to help employees improve their health; if...
Read MoreFrequently Asked Questions about Grandfathered Plans
As employers determine their plan designs for the coming year, those with grandfathered status need to decide if maintaining grandfathered status is their best option. Innovative, in conjunction with our Partner firm United Benefit Advisors, has created an FAQ to address the questions employers have about grandfathering a group health...
Read MoreEssential Health Benefits, Minimum Essential Coverage, Minimum Value Coverage – What’s The Difference?
The Patient Protection and Affordable Care Act (PPACA) uses terms that sound alike for three very different things. Here’s a closer look at these terms, and when they’re used. Essential Health Benefits Significantly affects individuals and small employers with a fully insured plan. Has a limited impact on self-funded and...
Read MoreUpdate: Same-Sex Marriages and Group Health Benefits
On October 6, 2014, the Supreme Court of the United States declined to review seven cases in which the lower appeals court had ruled that a state law or constitutional provision that prohibited same-sex marriage was unconstitutional. This declination means that the ruling of the appeals court is law, and...
Read MoreCompliance Alert! Deadline Approaching for Larger Self-Funded Health Plans To Obtain a Health Plan Identifier Number
To meet federal requirements, large health plans must obtain a national health plan identifier number (HPID) by November 5, 2014. For this requirement, a large health plan is one with more than $5 million in annual receipts. The Department of Health and Human Services (HHS) has said that since health...
Read MoreIRS Notice Addresses Handling of Changes in Measurement and Stability Periods
Large employers (for 2015, this generally means those with 100 or more full-time or full-time equivalent employees) may use either the monthly or look-back method to determine whether an employee on average works 30 or more hours per week, and for whom a penalty may be owed if adequate health...
Read MoreExcepted Benefits – “Limited Scope” Dental and Vision Plans and EAPs
On September 26, 2014, the U.S. Department of Health and Human Services (HHS), the Internal Revenue Service (IRS), and the Department of Labor (DOL) released final regulations that explain when dental and vision plans and employee assistance plans (EAPs) will be considered “excepted benefits.” Excepted benefits are health benefits that are...
Read MoreIRS Allows Additional Section 125 Change in Status Events
On September 18, 2014, the Internal Revenue Service (IRS) issued Notice 2014-55 which allows employers to amend their Section 125 plans to recognize several new changes in status events. Open Enrollment in the Health Insurance Marketplace Prior to this new notice, an opportunity to enroll in the health insurance Marketplace (or...
Read MoreOur September Educational Events were a Tremendous Success!
Our Innovative team presented an educational seminar at DelFrisco’s Double Eagle Steakhouse in Philadelphia on September 19th, and also at Fleming’s Steakhouse in Marlton on September 25th. The events, which introduced innovative solutions for controlling the costs within your health plan while complying with PPACA, attracted C-level executives as well...
Read MoreIRS Issues Drafts of Instructions for Employer and Individual Responsibility Reporting Forms
The following is a summary of draft instructions. Some of this information may change when the final forms and instructions are released. In order for the Internal Revenue Service (IRS) to verify that individuals have the required minimum essential coverage, individuals who request premium tax credits are entitled to them,...
Read MoreFrequently Asked Questions about the Transitional Reinsurance Fee (TRF)
The transitional reinsurance fee (TRF) applies to fully insured and self-funded major medical plans for 2014, 2015, and 2016. The purpose of the fee is to provide funds to help stabilize premiums in the individual insurance market in view of uncertainty about how the Patient Protection and Affordable Care Act...
Read MoreGroup Health Plan Notices: What Do You Need To Include?
Employers that sponsor group health plans are required to give eligible employees a number of notices each year. Some notices must be given by a particular date, and some must be given as part of the enrollment packet. (This means that non-calendar year plans may need to provide Medicare Part...
Read MoreHighlights of the Summary of Benefits and Coverage Requirement
Plan administrators of group health plans, which includes all employers regardless of size or type of business with the exception of those that have been grandfathered, must provide a Summary of Benefits and Coverage (SBC) to eligible individuals. This requirement applies primarily to medical (PPO, HDHP, HMO, etc…) coverage. There...
Read MoreIRS Issues Drafts of Individual Responsibility Reporting Forms
The following is a summary of draft forms. Some of this information may change when final forms, and the instructions, are released. In order for the IRS to verify that individuals and employers are meeting their shared responsibility obligations, and that individuals who request premium tax credits are entitled to...
Read MoreA September Lunch Event Is On The Calendar!
On February 10, 2014, the IRS issued final regulations on the employer requirements, often known as “Play or Pay.” For some employers Play or Pay is delayed until 2016, for others, compliance is still required in 2015. Make sure you know where you stand. Please join us on Friday September...
Read MoreCost of Living Adjustments for 2015
Many of the thresholds in PPACA have annual cost-of-living adjustments. The IRS has released the 2015 “affordability” thresholds. Affordability is measured differently for purposes of eligibility for the premium tax credit/subsidy (and any employer-shared responsibility penalty triggered by an employee receiving a premium subsidy) and the individual-shared responsibility penalty. For...
Read MoreCourts Issue Opposite Rulings in PPACA Subsidies Cases
On July 22, 2014, two Courts of Appeals issued decisions that address whether only people who live in states that have state-run Marketplaces (which are also called exchanges) are eligible to receive premium tax credits or subsidies under the Patient Protection and Affordable Care Act (PPACA). One court held that...
Read MoreAdditional Rules on Contraceptive Coverage
Following up on the Supreme Court’s decision in the Hobby Lobby case, the Departments of Labor, Health and Human Services, and Treasury have issued an FAQ that reminds employers that ERISA requires that plan participants be advised of a material reduction in benefits within 60 days after the reduction becomes effective....
Read MoreWill Your Private Plan Owe an MLR Rebate This Year?
MLR Rebate Considerations – Private Plans As was the case last year, insurers with medical loss ratios (MLRs) that were below the prescribed levels on their blocks of business must issue rebates to policyholders. Insurers must pay rebates owed on calendar year 2013 experience by August 1, 2014. The rules...
Read MoreWill Your Government or Church Plan Owe an MLR Rebate This Year?
MLR Rebate Considerations – Government and Church Plans As was the case last year, insurers with medical loss ratios (MLRs) that were below the prescribed levels on their blocks of business must issue rebates to policyholders. Insurers must pay rebates owed on calendar year 2013 experience by August 1, 2014....
Read MoreThe Federal Court of Appeals Says Subsidies for Obamacare are Illegal!
After an in-depth, careful reading of the Affordable Care Act, the Federal Appeals Court panel ruled 2-1 that government subsidies used to purchase health insurance on HealthCare.gov are illegal. The ruling stated that only exchanges that are run by an individual state, or the District of Columbia, are permitted to...
Read MoreFourth Circuit Court Says Subsidies in the Federal Exchange Are Legal
We now have a decision from another Court of Appeals (this time it’s the Fourth Circuit) on the exact same subsidy issue as posted earlier today. This court has held that it is legal for individuals enrolled in federally-run exchanges to receive subsidies. If this decision ultimately prevails, employers would...
Read MoreWhy HSAs Linked to HDHPs are Making a Comeback
According to new information from United Benefit Advisors (UBA), health savings accounts (HSAs) are outpacing health reimbursement arrangements (HRAs) in both adoption and participation rates. And now that metal tier health plans [e.g., platinum, gold, silver, etc.] are allowed higher deductibles, employers are increasingly looking at HSA qualified plans for...
Read MoreFollow-Up to the Hobby Lobby Decision
The Supreme Court of the United States recently decided in a case generally referred to as the Hobby Lobby case that closely-held corporations whose owners have religious objections to providing coverage for contraceptives are not required to provide that coverage to satisfy PPACA requirements. We still do not know how...
Read MoreWhat Does July 31st Mean To You?
Form 5500 With the exception of government plans (including most public schools) and many church plans which are exempt, plans on a calendar year that must comply with ERISA must file Form 5500 by July 31st. This form is part of ERISA’s overall reporting and disclosure framework, which is intended...
Read MoreWhat Employers Need to Know about SCOTUS Hobby Lobby Ruling
On June 30, 2014 the U.S. Supreme Court issued a decision in a case generally referred to as the Hobby Lobby case. Hobby Lobby is a family-owned for-profit corporation. The family that owns Hobby Lobby strongly believes that it would violate their deeply held religious values and obligations to provide...
Read MoreInnovative Receives Rave Reviews Once Again!
Last Friday at Sullivan’s Steak House in King of Prussia, our Innovative team revealed the three greatest concerns of our market regarding PPACA at an educational seminar lunch event. In speaking with clients and other employers in the area, it became clear that guidance is needed not only on compliance,...
Read MoreHow Does the New Orientation Period Affect the 90-Day Waiting Period?
The DOL recently (June 25, 2014) issued additional regulations regarding an Orientation Period for Employers. This Orientation Period is meant to provide both employer and employees alike the opportunity to evaluate whether the employment situation is satisfactory for each party. This period can occur prior to the start of the maximum...
Read MoreThe New Jersey Athletic Conference Board Invites Innovative As Their First Guest Speaker!
On Wednesday June 18th, Innovative’s Ryan Kastner, Employee Benefits Consultant, and Scott Agostini, Managing Director, were invited to speak at the NJAC (New Jersey Athletic Conference) semi-annual Board of Athletic Directors meeting in Atlantic City, where they educated the attendees on the possible effects of Health Care Reform to their...
Read MoreWhat Are The Final Regulations For PPACA’s Mandatory Reporting?
On September 5, 2013, the IRS issued proposed rules implementing the information reporting requirements under Code Sections 6056 and 6055. These proposed rules reflected a potential massive and duplicative amount of paperwork required by employers to comply with the reporting requirements of PPACA. On March 10, 2014, the IRS issued...
Read MoreNew Model COBRA Notices Should Be Used By Employers
The Department of Labor has published new model COBRA notices that reflect that coverage is available in the public health insurance exchanges and include information on special enrollment rights. Key points: • Employers should utilize the revised model notices. • Employers should be proactive in communicating with employees about “Marketplace”...
Read MoreHighlights of the Patient Centered Outcomes (PCORI) Comparative Effectiveness Fee
Updated June 2014 The Patient-Centered Outcomes Research Institute (PCORI) fee applies from 2012 to 2019. The fee is due based on plan/policy years ending on or after October 1, 2012, and before October 1, 2019. The fee is due by July 31 of the year following the calendar year in...
Read MoreDon’t Miss Our Next Seminar Lunch Event in King of Prussia!
PPACA Strategies- Innovative Solutions to Control Your Bottom Line With the passing of the Patient Protection and Affordable Care Act, CEO’s and CFO’s have never paid more attention to employee benefits than they are now. Please take advantage of the opportunity to be the most informed person in the room!...
Read MoreDo You Have The Correct Form To File Your PCORI Fees?
The Patient-Centered Outcomes Research Institute (PCORI) fee is imposed on insurers and plan sponsors of self-insured group health plans, with plan years ending after September 30, 2012 and before October 1, 2019. Sponsors of calendar year plans are required to pay the annual fee by July 31 of each year...
Read MoreSearching For Answers? Find Out How Your Company Compares
Don’t Miss Your Chance To Participate In The Largest Health Plan Benchmarking Survey In The Country! End your search for answers by participating in the 2014 UBA Health Plan Benchmarking Survey…and you will automatically be entered in a raffle to win the new iPad Air!!! Your survey needs to be...
Read MoreCOMPLIANCE ALERT! Self-Funded Health Plans Must Obtain a Health Plan Identifier Number
To meet federal requirements large health plans must obtain a national health plan identifier number (HPID) by November 5, 2014. For this requirement, a large health plan is one with more than $5 million in annual receipts. The Department of Health and Human Services (HHS) has said that since health...
Read MoreHow Does COBRA Affect Marketplace Enrollment?
The Obama Administration announced last week that workers who are eligible to continue health insurance coverage through COBRA (Consolidated Omnibus Budget Reconciliation Act), will now have the option of purchasing a plan through the Health Insurance Marketplace without having to wait until open enrollment. In many cases, workers will be...
Read MoreJoin Us For Our Lunch ‘N Learn May 16th: Managing Benefit Costs In The Health Care Reform Era
On February 10, 2014, the IRS issued final regulations on the employer-shared responsibility requirements, often known as “Play or Pay.” For some employers Play or Pay is delayed until 2016, for others, compliance is still required in 2015. Where do you stand? Please join us for a sizzling lunch where...
Read MoreInnovative Exhibits at the 28th Annual Tri-State HRMA Conference!
It was a “hole-in-one” day at the Westin in Mount Laurel on May 1st where about 250 attendees, and numerous exhibitors, came together for a day of education, networking and fun! Innovative Consultants Ryan Kastner, Dan Foley and Matt Bernstein, along with our Managing Director Scott Agostini, challenged attendees to...
Read MoreCost-Of-Living Adjustments for Health Savings Accounts (HSAs)
The IRS has issued the 2015 cost-of-living and coverage adjustments for HSAs. All limits have increased for 2015 as follows: Annual contribution limitation: Individual $3,350 (up from $3,300) Family $6,650 (up from $6,550) Annual Maximum Out-Of-Pocket Limits for HDHP*: Individual $6,450 (up from $6,350) Family $12,900 (up from $12,700) Annual...
Read MoreProposed Regulation: Health Plans Participating in the Exchange Must Provide a 90-Day Grace Period for Subsidized Coverage
For those individuals that purchase a subsidized health insurance plan through the Exchange, and have previously paid at least one full month’s premium during the benefit year, the insurance plan must provide for a 90-day grace period for premium payment before canceling for non-payment. Within this 90-day period, claims for...
Read MoreJoin Us At The 32nd Annual PEBA Forum On April 24th!
Innovative is looking forward to being an exhibitor at the 32nd Annual PEBA (PennJerDel Employee Benefits & Compensation Association) Forum this month, on Thursday April 24, 2014. The event will take place at the Hilton on City Line Avenue and is expecting an attendance of more than 300 compensation, benefit...
Read MoreRegulation Update: House Votes Full-Time As 40 Hours!
In a House vote of 248 to 179 last Thursday, the definition of full-time employee under The Patient Protection and Affordable Care Act (PPACA) was changed from 30 hours per week back to 40 hours per week. The bill was sponsored by Rep Todd C. Young, a Republican from Indiana. ...
Read MoreSearching For Answers? Find Out How Your Company Compares
Don’t Miss Your Chance To Participate In The Largest Health Plan Benchmarking Survey In The Country! End your search for answers by participating in the 2014 UBA Health Plan Benchmarking Survey…and you will automatically be entered in a raffle to win the new iPad Air!!! Your survey needs to be...
Read MoreIRS Releases Final Reporting Regulations
In order for the Internal Revenue Service (IRS) to verify that individuals and employers are meeting their shared responsibility obligations and that individuals who request premium tax credits are entitled to them, employers and issuers will be required to provide reporting on the health coverage they offer. The reporting requirements...
Read MoreOption for Some to Renew Policies That Do Not Fully Meet PPACA Standards
On March 5, 2014, the Department of Health and Human Services (HHS) released a Bulletin that allows state insurance departments to permit the renewal through October 1, 2016, of individual and small group policies that do not meet the “market reform” requirements of the Patient Protection and Affordable Care Act...
Read MoreThe Deadline Is Just A Few Weeks Away…
The Individual Mandate went into effect January 1, 2014. Compliance for this mandate requires that non-exempt U.S. citizens and legal residents must purchase and maintain “minimum essential coverage” which includes: • Individual market plans offered within a state, whether through or outside the Exchange • Eligible employer-sponsored plans • ...
Read MoreIt Was A Busy Month At Innovative With Two Outstanding Lunch Events and a Gala!
We did not let the snow get in our way in February! The month started off with _ Mark Sulpizio, Innovative Investment Fiduciaries, LLC Principal _, guiding attendees through the Retirement Fee Disclosure Regulations that went into effect in 2012 at a fantastic Seminar Lunch Event at McCormick & Schmick’s...
Read MoreDon’t Miss Your Chance To Participate In The Largest Health Plan Benchmarking Survey In The Country!
End your search for answers by participating in the 2014 UBA Health Plan Benchmarking Survey…and you will automatically be entered in a raffle to win the new iPad Air!!! With close to 11,000 employers participating in 2013, Innovative Benefit Planning, in conjunction with United Benefit Advisors (UBA), annually conducts the...
Read MoreFinal Regulations Issued on Eligibility Waiting Periods
On February 20, 2014, the Department of Health and Human Services (HHS), the Department of Labor (DOL) and the Internal Revenue Service (IRS) released final regulations on the eligibility waiting period requirements. The Patient Protection and Affordable Care Act (PPACA) provides that plans may not require an employee who is...
Read MoreFinal Regulations on Play or Pay: Non-Calendar Year Plans and Next Steps for Employers
Non-Calendar Year Plans Large employers with non-calendar year plans do not have to provide coverage until the start of the 2015 plan year, but the plan year effective date applies only if they meet a number of requirements. The most significant of these are: The employer had a group health...
Read MoreFinal Regulations on Play or Pay: Large Employer Responsibilities and Potential Penalties
If an employer is large enough for the play or pay requirements to apply (100 or more full-time or full-time equivalent employees for 2015 and 50 or more full-time or full-time equivalent employees for 2016 and beyond), two separate requirements, and potential penalties, apply. Full-time continues to mean 30 or...
Read MoreFinal Regulations on Play or Pay: Delay for Some Employers, and Who Is “Large”?
On February 10, 2014, the IRS issued final regulations on the employer-shared responsibility requirements, often known as “play or pay.” This is the requirement that large employers offer adequate coverage to their full-time employees or pay penalties. The final regulations follow the proposed regulations (which were issued in January 2013)...
Read MoreCompliance Alert! Employer Mandate Delayed For Some Employers
The Obama administration announced Monday February 10, 2014 yet another delay in the Employer Mandate portion of PPACA. The first delay pushed the requirement back to 2015 for all “large” employers, meaning those with over 50 employees. This new delay states that companies with 50-99 employees will not have to...
Read MoreCongratulations to Dan Foley and Ryan Kastner!
A key component of Innovative’s 2014 Strategic Plan is Focusing on improving Ourselves, Client situations and Innovative (FOCI). Dan Foley and Ryan Kastner embraced the initiative of self-improvement by completing the 13 modules of training classes and passing a rigorous examination to earn the designation of Certified Corporate Wellness Specialist®...
Read MoreThe 2014 UBA Health Plan Benchmarking Survey Is Open!
End your search for answers by participating in the 2014 UBA Health Plan Benchmarking Survey…and you will automatically be entered in a raffle to win the new iPad Air!!! With close to 11,000 employers participating in 2013, Innovative Benefit Planning, in conjunction with United Benefit Advisors (UBA), annually conducts the...
Read MoreWellness Program Clarifications: Tobacco and Outcome-Based Alternatives
Additional PPACA clarifications were released by the HHS and DOL on January 9, 2014 through an FAQ. Here are the updates you need to know concerning your Wellness Program: Wellness Programs The FAQ states that a plan that offers an annual opportunity to receive an incentive for non-use of tobacco...
Read MorePPACA Update: Mental Health And Substance Abuse
A recent FAQ was released by the DOL and HHS to clarify certain regulations within PPACA. Here is the update on mental health and substance abuse disorders: Mental Health and Substance Abuse Disorders Coverage for mental health and substance use disorder services are an EHB, so non-grandfathered individual and small...
Read MorePPACA Update: Expatriate Plans, Fixed Indemnity Policies (Individual Market) and Volunteer Firefighters
Recent clarifications became available from the HHS and DOL regarding several PPACA regulations. Below are the updates for Expatriate Plans, Fixed Indemnity Policies, and Volunteer Firefighters. Expatriate Plans Insured expatriate plans do not need to comply with most PPACA provisions. The FAQ clarifies that a plan is considered an insured...
Read MoreNew Update To Coverage Under “Preventive Care”
On January 9, 2014, the Department of Health and Human Services (HHS), the Department of Labor (DOL) and the Department of the Treasury (IRS) issued clarification on several outstanding issues within PPACA through an FAQ. Here is what is new for preventive care: Preventive Care The requirement that non-grandfathered plans...
Read MoreNew Clarifications On Out-of-Pocket Maximums Under PPACA
On January 9, 2014 the HHS and DOL issued a new FAQ that addressed issues outstanding under PPACA. Here is the update for out-of-pocket maximums: Out-of-Pocket Limits The FAQ clarifies that, for non-grandfathered plans, the out-of-pocket maximum: Must include deductibles, coinsurance and copayments for essential health benefits (EHBs). A plan...
Read MoreDo You Know When To Use A Wrap Around Plan Document Or Wrap Around SPD?
The Employee Retirement Income Security Act of 1974 (ERISA) regulates employee pension plans and welfare benefit plans, with the exception of government and church plans. It is required by ERISA that plan sponsors describe the terms and conditions of its welfare benefit plans on an official written plan document that...
Read MoreDo You Have Questions About Eligibility Waiting Periods? You Are Not Alone!
The 90-day maximum for eligibility waiting periods is effective as of the start of the 2014 plan year. As employers are beginning to implement this new requirement, many have questions. Together with United Benefit Advisors (UBA), we have created a PPACA Advisor that addresses a number of recurring questions about...
Read MoreW-2 Reporting in 2014: Do You Have To Report Your Health Plan Costs, Or Not?
Employers that issued 250 or more W-2s in 2012 will need to include the cost of health coverage provided to an employee during 2013 on the employee’s W-2. Unlike most PPACA requirements, the 250 W-2 threshold is based on each employer’s situation, not the entire controlled group. The rules have...
Read MoreWhat Are Excepted Benefits?
“Excepted benefits” are health benefits that are limited in some way, such as stand-alone dental, long-term care, hospital indemnity, and Medicare supplement policies. Excepted benefits do not need to meet all of the PPACA requirements and they are not considered “minimum essential” benefits. The agencies have proposed three changes to...
Read MoreWho Will Be Paying An Additional Medicare Tax?
The IRS issued final regulations on the additional 0.9 percent Medicare tax owed by high earners beginning in 2013. Employers must withhold this additional 0.9 percent from the employee’s pay only (there is no employer “match”) once the employee’s pay exceeds $200,000. If you would like a White Paper on...
Read MoreWhat are the Projected 2015 Figures ?
HHS and the IRS released anticipated 2015 figures, including: A transitional reinsurance fee (TRF) of $44 (down from $63 for 2014) Maximum out-of-pocket (OOP) expenses of $6,750 for single coverage and $13,500 for family coverage (up from $6,350 and 12,700 respectively for 2014) A deductible maximum in the small group...
Read MoreFrequently Asked Questions About The W-2 Reporting Requirement
Employers that issued 250 or more W-2s in the prior calendar year must include the value of “employer-sponsored group health coverage” on their employees’ W-2s. This means that an employer that issued 250 or more W-2s during 2012 must include the value of employer-sponsored coverage on the employee’s 2013 W-2...
Read MoreWho Is Eligible For The Small Business Tax Credit?
Beginning in 2014, the small business tax credit will only be available to small employers that offer coverage through the SHOP marketplace. Several counties in Washington and Wisconsin will not have SHOPs available in 2014, however. In Notice 2014-6, the IRS states that employers located in those counties will still...
Read MorePre-Existing Condition Insurance Plan Extended
HHS has announced that the Pre-Existing Condition Insurance Plan (PCIP) also has been extended through January 31, 2014. The PCIP will be replaced by marketplace coverage, but to accommodate PCIP enrollees who have not been able to obtain coverage through the marketplace, the PCIP is being extended for one month....
Read MoreHHS Announces Extensions to Enrollment and Premium Deadlines for Marketplace Coverage
The U.S. Department of Health and Human Services (HHS) recently released an Interim Final Rule that formally extends some of the marketplace (also known as the exchange) deadlines and encourages insurers to provide additional extensions if possible. Extensions Affecting the Federally-Facilitated Small Business Health Options Program (FF-SHOP) Marketplace The rule...
Read MoreNew Option for Individuals Who Have Lost Coverage to Purchase a Catastrophic Policy
Currently, catastrophic coverage only is available in the marketplace to people under age 30 and to those who do not need to meet the individual mandate either because the cost of coverage exceeds eight percent of household income or they qualify for a hardship exemption. Catastrophic plans generally will cover...
Read MoreIRS Issues Notice about Same-Sex Spouses under Section 125 Plans, Flexible Spending Accounts, and Health Savings Accounts
On Dec. 16, 2013, the Internal Revenue Service (IRS) issued Notice 2014-1 which provides some answers about covering same-sex spouses under Section 125 plans in light of the Windsor decision. In the Windsor decision, the U.S. Supreme Court ruled that the part of the Defense of Marriage Act (DOMA) that prohibited...
Read MoreDo You Understand the 2014 Requirements for Your Wellness Program?
The wellness program rules provide an exception to the general rule that employers may not take a person’s health status into account with respect to eligibility, benefits, or premiums under a group health plan. Wellness programs, therefore, are allowed if they are designed to help employees improve their health; if...
Read MoreMaximum Deductible for 2015 – Affects Small Employers With Fully Insured Plans
HHS has announced that it expects that in 2015 the maximum deductible for insured small group plans will be $2,150 for employee-only coverage and $4,300 for family coverage (up from $2,000 and $4,000 respectively for 2014).* While there may be modifications when the final notice is released, the figures likely...
Read MoreChanges Affecting Small Insured Plans
Beginning in 2015, if an insurer agrees to use a composite rate, the rate could not be changed during the year, even if the composition of the group changes. Insurers are encouraged to follow this practice during 2014. This applies both inside and outside the SHOP marketplace. The HHS actuarial...
Read MoreTransitional Reinsurance Fee – Affects Large and Small Employers, Whether Fully Insured or Self-Funded
The Internal Revenue Service (IRS) and the Department of Health and Human Services (HHS) recently issued an update on the Transitional Reinsurance Fee (TRF) as follows: A Transitional Reinsurance Fee (TRF) will be assessed on both insured and self-funded plans for the 2014, 2015, and 2016 calendar years to help...
Read MoreOpen Enrollment for the Marketplaces – May Affect Large and Small Employers, Whether Fully Insured or Self-Funded
Open enrollment for the individual marketplaces for 2015 coverage will run from Nov. 15, 2014, through Jan. 15, 2015. Coverage would begin on Jan. 1, 2015, for individuals enrolling from Nov. 15 through Dec. 15, 2014, and on Feb. 1, 2015, for those enrolling from Dec. 16, 2014, through Jan....
Read MoreMaximum Out-of-Pocket for 2015 – Affects Large and Small Employers, Whether Fully Insured or Self-Funded
HHS has announced that it expects that the maximum out-of-pocket limit for non-grandfathered plans in 2015 to be $6,750 for employee-only coverage and $13,500 for family coverage (up from $6,350 and $12,700 respectively for 2014). While it is possible that there will be modifications when the final notice is released,...
Read MoreMental Health Parity and Addiction Equity Act of 2008 – Key Clarifications Made By Final Regulations
The Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) seeks to ensure that medical plans, including group health plans, that provide mental health and substance use disorder benefits do so in a manner that generally is on par with the medical benefits offered under the plans. The MHPAEA...
Read MoreOur November Lunch Events Were A Huge Success!
Guests at our Fiduciary Best Practices lunch event that was held at DelFrisco’s Double Eagle Steakhouse in Philadelphia on November 14th learned more about the fee disclosure regulations that went into effect in 2011. Innovative’s own Mark Sulpizio discussed how to better understand the fee disclosures provided and address what...
Read MoreInsurers Given Permission to Renew Policies That Don’t Meet PPACA Requirements
Yesterday (Nov. 14, 2013) the White House announced that insurers will not be required to meet most of the provisions of the Patient Protection and Affordable Care Act (PPACA) if they renew individual or small group policies that were in effect on Oct. 1, 2013. The Department of Health and...
Read More2014 Cost-Of-Living Adjustments for Health Plans, Section 125 Plans and Social Security/Medicare
Many employee benefit limits are automatically adjusted each year for inflation (this is often referred to as an “indexed” limit). The Internal Revenue Service and the Social Security Administration have released the indexed figures for 2014. Because inflation is relatively low and some amounts are adjusted only if the increase...
Read MoreUBA’s Private Exchange “Benefits Passport” Is Now Open!
Employers, are you looking for an affordable insurance option to help reduce your costs, increase efficiency, simplify administration and provide exceptional value to your employees in light of Health Care Reform? Your search is over. United Benefit Advisors (UBA), the nation’s leading independent employee benefits advisory organization, announced yesterday the...
Read MoreHealth FSA “Use-It-Or-Lose-It” Rule Modified
What some would consider a long overdue change to FSA plans came down from the US Department of Treasury yesterday. The FSA “use-it-or-lose-it” provision, which has required employees to spend pre-tax dollars set aside for certain medical expenses by the end of the year or forfeit those funds, was put...
Read MoreSelf-Funded Employers Get Some Relief: Pay Only 2014 Transitional Reinsurance Fee!
Some employers with self-funded health plans can breathe a sigh of relief this week. The Department of Health and Human Services has announced that certain self-funding employers will be exempt from paying the second and third year Transitional Reinsurance Program Fees imposed by the Affordable Care Act. The first year...
Read MoreHealth Plan Benchmarking Regional Findings: How Does Your Plan Compare?
The benefits landscape remains in a state of flux as the cost of health care continues to increase and recruitment and retention of quality employees becomes more competitive. Combined with the potential impact from Health Care Reform legislation, employers are increasingly challenged to find accurate information that will help them...
Read MoreIs Eligibility For The Marketplace A Section 125 Change In Status Event For Non-Calendar Year Plans?
With the October 1st opening of the Health Insurance Marketplace, some employers have inquired about where they stand if an employee would like to leave their plan. In particular, those employers with a non-calendar year Section 125 plan have asked for guidance on whether entering the Exchange is considered a...
Read MoreBoiling Down PPACA
We’ve had a lot of employers request a simple, at-a-glance way to see all the PPACA requirements that apply to their business. This is no easy task given group size, SHOP exchanges and self-funding variables! Let’s just look at a few provisions that are effective for the plan year beginning...
Read MoreHow Does Your Health Plan Stack Up Against Your Competitors?
See how your health plan stacks up against your competitors! Results from the United Benefit Advisors (UBA) 2013 Health Plan Survey are in! Employers can now benchmark their health plan costs and design against the nation’s largest health plan benchmarking survey of nearly 11,000 respondents. to receive a Benchmarking report...
Read MoreNew Guidance on HRAs and Premium Reimbursement Arrangements
On Sept. 13, 2013, the IRS issued Notice 2013-54, which includes details on permissible health reimbursement arrangements (HRAs), provides some clarification on minimum essential, minimum value and affordable coverage, and addresses payment of individual premiums through an employer-provided plan. HRAs Most people had expected that standalone HRAs would have difficulty...
Read MoreWhat Is A “Common Law Employee?”
As part of PPACA, every employer needs to determine whether or not they are “large” which, according to Health Care Reform, means employing 50 or more full time or full-time equivalent employees. Who exactly does this include? Contractors? While there is no set definition of a “Common Law” employee, there...
Read MoreGOVERNMENT SHUTDOWN – NOW WHAT?
The failure of the U. S. Senate and House of Representatives to agree on a new budget for the Fiscal Year (beginning October 1) is resulting in a furlough of more than 800,000 federal workers and government agencies temporarily closing or cutting back the operations of numerous federal facilities and...
Read MoreIRS Provides Process to Correct Over-Withholding of Same-Sex Spouse Benefits
On Sept. 23, 2013, the IRS issued Notice 2013-61. This notice provides a special process for employers to make refund claims or internal adjustments of FICA and federal income tax (FIT) that was withheld or paid in connection with same-sex spouse benefits. Employers that prefer to use the normal refund...
Read MoreHighlights of the SHOP Exchange
PPACA requires that a Small Business Health Options Program (SHOP) exchange/marketplace be established in each state for small employers. For 2014, all states will use 50 employees as the cut-off for small employer status.* Beginning in 2016, all states must use 100 employees as the cut-off. The SHOP exchanges/marketplaces will...
Read MoreDOL Announces Non-Enforcement of Marketplace/Exchange Notice
PPACA requires employers covered by the Fair Labor Standards Act to provide a notice about the upcoming health marketplaces (also called exchanges) to their employees. The notice is due Oct. 1, 2013. On Sept. 11, 2013 the Department of Labor (DOL) announced that it will not penalize employers that do...
Read MoreA Delay for Out-Of-Pocket Maximums
A few weeks ago several media outlets picked up a FAQ that the Department of Labor issued in February of this year. The FAQ may be accessed here: FAQs About Affordable Care Act Implementation Part XII Some of the reports have created confusion about the requirement, and the scope of...
Read MoreIRS Releases Proposed PPACA Reporting Rules
On Sept. 5, 2013, the Internal Revenue Service (IRS) released the long-awaited rules that describe the reporting that plans, employers, and insurers will need to provide in support of the individual shared-responsibility and employer shared-responsibility requirements of the Patient Protection and Affordable Care Act (PPACA). The rules are proposed, so...
Read MoreHighlights of Exchange Notice Requirement
Most employers must give a notice about the upcoming health exchanges/marketplaces to all existing employees by Oct. 1, 2013. Employees hired after that date must receive the notice within 14 days following their start date. All employers who are subject to the Fair Labor Standards Act must give the notice....
Read MoreFrequently Asked Questions about the Exchange (Marketplace) Notice
This FAQ is based on Department of Labor (DOL) Technical Release 2013-02, which does not provide specific guidance on many issues. Consequently, some of the answers in this FAQ are based on agency guidance provided in similar situations. The answers in this FAQ assume the employer is completing the model...
Read MoreIRS Issues Rules on Same-Sex Marriages
On Aug. 29, 2013, the IRS issued Revenue Ruling 2013-17, which describes how the IRS will handle same-sex marriages for federal tax purposes in light of the U.S. Supreme Court decision that found a part of the Defense of Marriage Act (DOMA) unconstitutional. The ruling says: The IRS will consider...
Read MoreThe October 1st Deadline Is Just Around The Corner: Employers Must Provide Notices Regarding Availability of Exchange Coverage
A provision of the 2010 health care reform law requires employers to provide notices to all employees regarding the availability of health coverage options through the state-based exchanges created pursuant to that law. The DOL issued temporary guidance on May 8, 2013 (Technical Release 2013-02) and model notices for employers...
Read MoreThe Real Story on Out-Of-Pocket Maximums
Last week several media outlets picked up a FAQ that the Department of Labor issued in February of this year. The FAQ may be accessed here: FAQs about Affordable Care Act Implementation Part XII Some of the reports have created confusion about the requirement, and the scope of what has...
Read MoreFrequently Asked Questions About Grandfathered Plans – Part Two
Those employers with grandfathered status need to decide if maintaining grandfathered status is their best option for the coming year. Here is a continuation of the questions asked most frequently, and answers, about grandfathering a group health plan. Q5: How are changes measured? A5: Changes are measured cumulatively since March...
Read MoreFrequently Asked Questions About Grandfathered Plans – Part One
As employers determine their plan designs for the coming year, those with grandfathered status need to decide if maintaining grandfathered status is their best option. Following are some frequently asked questions, and answers, about grandfathering a group health plan. Q1: May plans maintain grandfathered status after 2014? A1: Yes, they...
Read MoreThe Individual Mandate: Noteworthy Numbers
For 2013: The tax filing threshold is $10,000 if filing single and $20,000 if married and filing jointly. Federal Poverty Level (FPL) in the 48 contiguous states is $11,490 for a single household and $45,960 for household of four. It is $14,350/29,440 in Alaska and $13,230/27,090 in Hawaii. The subsidy...
Read MoreIndividual Mandate: Who Is Eligible For Premium Subsidies?
To help lower-income people meet the requirement to have insurance, a premium subsidy will be available to a person who: Purchases coverage through a public marketplace/exchange; and Has a household modified adjusted gross income between 100 or 133 percent (depending on their state) and 400 percent of Federal Poverty Level...
Read MorePPACA And The Individual Shared Responsibility Requirement
Although the employer shared responsibility requirements have been delayed to 2015, the individual responsibility requirement (also known as the individual mandate) is still scheduled to take effect in 2014. Under the individual mandate, most people residing in the U.S. will be required to have minimum essential coverage, or they will...
Read MoreMLR REBATE CONSIDERATIONS – PRIVATE PLANS
As was the case last year, insurers with medical loss ratios (MLRs) that were below the prescribed levels on their blocks of business must issue rebates to policyholders. Insurers must pay rebates owed on calendar year 2012 experience by Aug. 1, 2013. The rules for calculating and distributing these rebates...
Read MoreMLR REBATE CONSIDERATIONS – GOVERNMENT AND CHURCH PLANS
As was the case last year, insurers with medical loss ratios (MLRs) that were below the prescribed levels on their blocks of business must issue rebates to policyholders. Insurers must pay rebates owed on calendar year 2012 experience by Aug. 1, 2013. The rules for calculating and distributing these rebates...
Read MoreIRS Confirms Play or Pay Delay
On July 9, 2013 the Internal Revenue Service issued Notice 2013-45, which confirms that the employer shared responsibility penalties and reporting requirements will not apply until 2015. Last week the Department of the Treasury and the White House blogged that this announcement was coming. The IRS Notice states that employers...
Read MoreSpanish Version of Notice of Exchange is Now Available
The DOL has provided Spanish versions of the model notice regarding the exchange/health insurance marketplace. While employers are not specifically required to provide the Spanish version to Spanish-speaking employees, since the notice is supposed to be understandable by the average employee, providing the Spanish version where appropriate is advisable. There...
Read MorePlay or Pay Penalty Delayed To 2015
On July 2, 2013 the Department of the Treasury and the White House used their blogs to announce that the employer reporting requirements, and the employer shared responsibility/Play or Pay penalty, are being delayed until 2015. The Treasury said that it will provide a formal announcement and additional details next...
Read MorePPACA: Individual Grace Period
Effective Date for Individual Mandate Delayed For Some People On June 26, 2013 the IRS unexpectedly issued a notice that gives individuals who are eligible for coverage under an employer-sponsored health plan, but who have not elected coverage under that plan, until the start of the 2014 plan year to...
Read MoreU.S. Supreme Court Rules Legally-Married Same-Sex Spouses Entitled to Federal Recognition and Lifts California Ban on Same-Sex Marriage
The United States Supreme Court has issued two decisions that expand same-sex marriage rights. In the first, United States v. Windsor, No. 12-307 (June 26, 2013), the Court ruled unconstitutional a law denying federal recognition of legally-married same-sex couples. In the second, Hollingsworth, et al. v. Perry, No. 12-144 (June...
Read MoreThe 2013 UBA Health Plan Benchmarking Survey Has Closed And The Winner Of The iPad Is…
THE WINNER IS: The Philadelphia Zoo!!! We had an overwhelming response to our 2013 UBA Health Plan Benchmarking Survey and we are happy to announce that we have randomly picked the winner for the Apple 32 GB iPad! With over 18,000 plans participating, including more than 75 plans from our...
Read MoreHave You Made Any “Material Modifications” To Your Plan Since Your Last SBC Was Issued?
If a group health plan or health insurance issuer have made any material modification (during the plan year) in terms of the plan or coverage involved that’s not reflected in the most recent Summary of Benefits and Coverage (SBC), the plan or issuer must provide notice of the modification to...
Read MoreCOMPLIANCE ALERT!! Final “SHOP” Regulations Issued
On June 4, 2013, the Department of Health and Human Services (“HHS”), Centers for Medicare & Medicaid Services (“CMS”), issued final regulations implementing the provisions of the Affordable Care Act (“ACA”) related to the establishment and operation of the Small Business Health Options Program (“SHOP”). The final regulations delay by...
Read MorePCORI Fee Due Date
By July 31, 2013, most issuers of health insurance policies and plan sponsors of self-insured health plans must pay a fee of $1 per covered life as a result of new provisions in the Patient Protection and Affordable Care Act. The fee will partially fund the Patient-Centered Outcome Research Institute...
Read MorePPACA: Certificates of Creditable Coverage
Affects all plans, whether fully insured, self-funded or grandfathered, and regardless of employer size, as of Jan. 1, 2015. Because pre-existing condition limitations will not be permitted after the start of the 2014 plan year, certificates of creditable coverage would not need to be provided after Dec. 31, 2014. (This...
Read MoreAGENCIES ISSUE FINAL RULES ON WELLNESS PROGRAMS
On May 29, 2013 the Department of Health and Human Services, the Internal Revenue Service and the Department of Labor jointly issued a final rule that addresses how wellness programs must operate under PPACA beginning in 2014. In many respects the final rules carry forward the rules that have been...
Read MoreDo You Know What The Summary Of Benefits & Coverage Requirements Are Under Health Care Reform?
A Summary of Benefits & Coverage (SBC) is required starting the first day of the first plan year after September 23, 2012, or the first day of the first open enrollment period after this date. Health insurers and group health plans must provide the SBC and the Uniform Glossary to...
Read MoreCOMPLIANCE ALERT! Employers Must Provide Notices Regarding Availability of Exchange Coverage
A provision of the 2010 health care reform law requires employers to provide notices, by March 1, 2013, to all employees regarding the availability of health coverage options through the state-based exchanges created pursuant to that law. In January, the Department of Labor had announced delayed enforcement of the exchange...
Read MoreAN UPDATED SUMMARY OF BENEFITS AND COVERAGE FORM AND ANNUAL LIMITS WAIVERS
The agencies have released an updated Summary of Benefits and Coverage (SBC) template that plans will need to use for 2014. The updated template has very few changes from the version used for 2013. The primary change is that the 2014 SBC must state whether or not the plan provides...
Read MoreWellness Incentives and the Play or Pay Requirement
The Departments of Labor, Health and Human Services and the Treasury have issued several updates that affect employer-sponsored group health plans. Wellness Incentives, HRAs, Minimum Value and Affordability The IRS has released proposed regulations that address how wellness incentives or penalties are applied to premium affordability (for purposes of the...
Read MoreThe Department of Labor Begins Auditing Group Health Plans for PPACA, GINA and Wellness Program Compliance
Employers that have had their group health plans audited by the Employee Benefits Security Administration (EBSA, the arm of the U.S. Department of Labor that enforces Title I of ERISA) are aware of the broad nature of the document requests and compliance reviews carried out under these audits. The EBSA...
Read MoreCOMPLIANCE ALERT! Important Transition Relief for Non-Calendar Year Plans
The January 1, 2014 effective date of the Pay-or-Play requirements under health care reform presents special issues for employers with non-calendar year plans. Prior to the release of the proposed regulations under the shared responsibility rules, employers with non-calendar year plans would either need to comply with the Pay-or-Play requirements...
Read MoreEssential Health Benefits, Minimum Essential Coverage, Minimum Value Coverage – What’s The Difference?
The Patient Protection and Affordable Care Act (PPACA) uses terms that sound alike for three very different things. Here’s a closer look at these terms, and when they’re used. Essential Health Benefits Significantly affects individuals and small employers with a fully insured plan. Has a limited impact on self-funded and...
Read MoreEmployers, Do You Know What You Need To Do Before January 2014 To Comply With PPACA?
The provisions associated with health care reform pose many questions for employers, most importantly, what do I need to do and when? Here is a checklist of items to cross off your list before January 2014: Calculate and pay the Patient Centered Outcome Fee if the plan is self-funded (insurers...
Read MoreREGISTER NOW!! Health Care Reform Lunch ‘N Learn Events in Weehawken and Marlton
Since the November Presidential election, Innovative has hosted eight Lunch N’ Learn events in New Jersey, Pennsylvania and New York, and we have just added two more! We will be having our first Weehawken event at The Chart House Restaurant this month on April 24th, and we will be back...
Read MorePPACA Update: External Claims Appeals Requirement
Applies to all nongrandfathered plans, whether fully insured or self-funded, and to all sizes of employers. PPACA requires all nongrandfathered plans to follow detailed processes for claims appeals, including a process for external review that includes 16 consumer protections required under the NAIC model act. Due to practical difficulties meeting...
Read MoreTerriann to Speak about Health Care Reform at Tri-State HRMA’s 27th Annual Conference
Since the election in November, Terriann Procida has been educating employers about Health Care Reform, specifically the new Play or Pay regulation. Do you know what you need to do to begin budgeting for the 2013-2014 PPACA Provisions? Do you understand how potential penalties associated with Play or Pay may...
Read MorePPACA Update: Certificates of Creditable Coverage
Affects all plans, whether fully insured, self-funded or grandfathered, and regardless of employer size, as of Jan. 1, 2015. Because pre-existing condition limitations will not be permitted after the start of the 2014 plan year, certificates of creditable coverage would not need to be provided after Dec. 31, 2014. (This...
Read MorePPACA Update: Eligibility Waiting Periods
Affects all plans, whether fully insured, self-funded or grandfathered. Applies to all sizes of employers, as of the start of the 2014 plan year. The agencies have issued proposed regulations that state that an eligibility waiting period cannot be more than 90 days. This literally is 90 calendar days —...
Read MorePPACA Employer Fees: Patient-Centered Outcomes Research Institute (PCORI) and Transitional Reinsurance (TRF)
The IRS and the Department of Health and Human Services have issued final regulations that provide details on two new, temporary fees that will be due as part of the Patient Protection and Affordable Care Act (PPACA). These fees will be calculated and paid directly by self-funded plans. The fees...
Read MorePlay or Pay: Non-Calendar Year Transition Rules for Measuring in 2013
A non-calendar year plan that had coverage in place on Dec. 27, 2012: Will not owe the “inadequate coverage penalty” on any employee who was eligible for coverage on Dec. 27, 2012 (and on employees hired after that date, if they would have been eligible under the rules in effect...
Read MoreFinal Regulations Issued on Market Reforms-Fair Health Insurance Premiums for Fully Insured Health Care Plans
Impacts all non-grandfathered fully insured small group plans (both in and outside the exchange) beginning with the 2014 plan year: The changes in the rules that apply to fully insured small groups, whether the coverage is provided inside or outside the exchange, are significant. From an employer standpoint, the most...
Read MoreFinal Regulations Issued on Market Reforms-Guaranteed Access for Fully Insured Health Care Plans
Impacts all nongrandfathered fully insured plans, whether inside or outside the exchange, beginning with the 2014 plan year: Guaranteed issue and renewal will apply to all insured plans regardless of size. Participation and employer contribution requirements will not be permitted under the guaranteed availability rules, although insurers may impose participation...
Read MoreFinal Regulations Issued on Essential Benefits and Actuarial Value for Fully Insured Health Care Plans
Impacts non-grandfathered small-group plans (both in and outside the exchange) beginning with the 2014 plan year: Beginning with the 2014 plan year all nongrandfathered plans in the small group market – whether inside or outside the exchange – will need to provide the “essential health benefits package” (EHB package). The...
Read MoreFAQ Released: Final Regulations Issued on Minimum Value for Self-Funded Health Care Plans
Impacts all self-funded plans as of the start of the 2014 plan year Self-funded plans (regardless of size) will not be required to provide the ten “essential health benefits” or coverage at a “metal level” as some plans will be required to do. (The essential health benefits are coverage within...
Read MoreFAQ Released: Final Regulations Issued on Minimum Value for Fully Insured Health Care Plans
Impacts large fully insured plans with 50 or more employees: Large group insured plans are not required to provide the ten “essential health benefits” or coverage at a “metal level” as small plans will be required to do. (The essential health benefits are coverage within these categories – ambulatory/outpatient, emergency,...
Read MoreCOMPLIANCE ALERT: Labor Department Releases New FMLA Model Forms and Notice Poster
The U.S. Department of Labor has released revised model Family and Medical Leave Act (“FMLA”) forms to administer federal FMLA leave and a notice poster. The updated forms should be used by employers immediately, although they include no substantive revisions despite recent rulemaking on the FMLA military caregiver leave provisions...
Read MoreSelf-Funded Health Care Plans FAQ Released: Final Regulations Issued on Out-of-Pocket Limits
Impacts all non-grandfathered self-funded plans beginning with the 2014 plan year The FAQ also talks about the out-of-pocket maximum requirements. Beginning with the 2014 plan year, plans may not have an out-of-pocket maximum that is larger than the allowed out-of-pocket limit for high-deductible health plans (HDHP) issued in connection with...
Read MoreFully Insured Health Care Plans FAQ Released: Final Regulations Issued on Out-of-Pocket Limits
Impacts all nongrandfathered fully insured plans beginning with the 2014 plan year: The FAQ also talks about the out-of-pocket maximum requirements. Beginning with the 2014 plan year, plans may not have an out-of-pocket maximum that is larger than the allowed out-of-pocket limit for high-deductible health plans (HDHP) issued in connection...
Read MoreSelf-Funded Health Care Plans FAQ Released: Final Regulations Issued on Preventive Care
Impacts all non-grandfathered, self-funded plans now: The agencies have received many questions about the requirement to provide first-dollar preventive care. They have now issued a FAQ that clarifies that: While plans generally do not need to provide out-of-network preventive care if there are no in-network providers able to provide the...
Read MoreFully Insured Health Care Plans FAQ Released: Final Regulations Issued on Preventive Care
Impacts all non-grandfathered fully insured plans now: The agencies have received many questions about the requirement to provide first-dollar preventive care. They have now issued a FAQ that clarifies that: While plans generally do not need to provide out-of-network preventive care if there are no in-network providers able to provide...
Read MoreFAQ Released: Final Regulations Issued on Whistleblowing for Self-Funded Health Care Plans
Impacts all self-funded plans beginning April 2013 PPACA prohibits employers (including insurers) from retaliating against an employee for reporting possible violations of PPACA to his employer or to the government, providing testimony about the possible violation or refusing to violate the law. It also prohibits retaliating or taking an unfavorable...
Read MoreFAQ Released: Final Regulations Issued on Whistleblowing for Fully Insured Health Care Plans
Impacts all fully insured plans beginning April 2013 PPACA prohibits employers (including insurers) from retaliating against an employee for reporting possible violations of PPACA to his employer or to the government, providing testimony about the possible violation or refusing to violate the law. It also prohibits retaliating or taking an...
Read MoreTerriann Scheduled to Speak about Health Care Reform at Tri-State HRMA’s 27th Annual Conference
Since the election in November, Terriann Procida has been educating employers about Health Care Reform, specifically the new Play or Pay regulation. Do you know what you need to do to begin budgeting for the 2013-2014 PPACA Provisions? Do you understand how potential penalties associated with Play or Pay may...
Read MorePPACA’s “Affordability” Requirement is Clarified by the IRS
The IRS finalized a rule that clarified that the health coverage “affordability” requirement (that an employee’s premium contribution not exceed 9.5 percent of household income) under the Patient Protection and Affordable Care Act (PPACA) will be based on self-only coverage, according to a Business Insurance online report. Employers with plans...
Read MorePPACA Update: Women’s Preventive Services
Proposed rules that would make it simpler for religious organizations and religious-affiliated not-for-profit organizations like hospitals and schools that have a religious objection to providing contraceptive services were released by the DOL on Feb. 1, 2013. These employers would notify their insurer of their objection, and the insurer automatically would...
Read MorePPACA Update: Minimum Essential Coverage
On Feb. 1, 2013, HHS and the IRS issued two proposed regulations that provide details on the individual shared responsibility requirement. PPACA requires that non-exempt individuals obtain “minimum essential coverage” or pay a penalty. Minimum essential coverage includes individual insurance, Medicare, Medicaid, CHIP, TRICARE, VA and similar government programs, and...
Read MorePPACA Update: IRS Issues Final Regulation on Tax Credits
On Feb. 1, 2013, the IRS issued a final regulation that provides the long awaited answer of whether family members of an employee who has access to affordable self-only coverage are eligible for a premium tax credit/subsidy. The answer is that they are not – if the employee has access...
Read MoreHRA Restrictions Under PPACA
Because PPACA prohibits annual dollar limits on essential health benefits, HRAs that are not integrated with other group health coverage (usually a major medical plan) will not be permitted after Jan. 1, 2014. The January 24, 2013 DOL FAQ states that an employer-provided HRA will not be considered integrated (and...
Read MorePPACA Update: Notice of Exchange Has Been Delayed
The Department of Health and Human Services (HHS), the Internal Revenue Service (IRS) and the Department of Labor (DOL) have recently issued more FAQs and proposed rules that address several employer obligations under the Patient Protection and Affordable Care Act (PPACA). On Jan. 24, 2013, the DOL issued a FAQ...
Read MoreCOMPLIANCE ALERT! Final HIPAA Privacy Regulations are Published
The Office for Civil Rights (“OCR”) of the U.S. Department of Health and Human Services published its long-awaited final privacy and security regulations (“Final Rule”) under the Health Insurance Portability and Accountability Act (“HIPAA”) on January 25, 2013. The Final Rule becomes effective March 26, 2013, and, in general, covered...
Read MoreWhat All Employers Need to Know About the “Cadillac Tax”
Starting in 2018, employers offering health plans that exceed a certain cost (the total employee and employer cost) would be subject to a 40% excise tax on the amount above that value. For individual coverage, the threshold would be $10,200 and for family coverage the threshold would be $27,500.* The...
Read MoreCoordinating Exchange and Plan Open Enrollments
On Jan. 2, 2013, the IRS issued a detailed rule that, among other things, provides that noncalendar-year plans may amend their Section 125 plans to allow employees to make midyear changes because of PPACA. Open enrollment for the exchanges will begin in October 2013 for a Jan. 1, 2014, effective...
Read MoreHow Will an Employer Know if an Employee Applies for a Premium Subsidy in the Exchange?
On Jan. 14, 2013, the Department of Health and Human Services (HHS) issued another lengthy proposed rule under the Patient Protection and Affordable Care Act (PPACA). Among other things, the proposed rule provides some information on how employers will be notified if an employee applies for a premium subsidy /...
Read MoreTerriann Presents to the Philadelphia Chapter of Women Presidents’ Organization!
As an area business owner herself, and an expert on Health Care Reform, Terriann Procida is honored to present “Health Care Reform: An Update on PPACA Since the Election” to the Philadelphia Chapter of Women Presidents’ Organization. The PPACA provisions present some challenges to employers in deciphering the new regulations...
Read MorePPACA: What Do Employers Need To Do Between Now And January 2014?
The provisions associated with health care reform pose many questions for employers, most importantly, what do I need to do and when? Here is a checklist of items to cross off your list before January 2014: Calculate and pay the Patient Centered Outcome Fee if the plan is self-funded (insurers...
Read MoreWhat Should Employers Already Be Doing To Comply With PPACA?
Plans: May not have a lifetime dollar maximum on any “essential health benefit” May not have an annual dollar limit on an “essential health benefit” that is over a certain amount Must cover the employee’s dependent children until the dependent reaches age 26 – even if the child...
Read MoreHealth Care Reform Update: IRS Proposes Regulations on Employer Penalty
The Internal Revenue Service has released proposed regulations on the health care reform employer “shared responsibility” penalty provision. This is the penalty on “large” employers (those with at least 50 full-time or full-time equivalent employees) that do not provide affordable minimum essential coverage for full-time employees and their dependents and...
Read MoreCompliance Alert! DOL Begins Auditing Group Health Plans for PPACA, GINA and Wellness Program Compliance
Employers that have had their group health plans audited by the Employee Benefits Security Administration (EBSA, the arm of the U.S. Department of Labor that enforces Title I of ERISA) are aware of the broad nature of the document requests and compliance reviews carried out under these audits. The EBSA...
Read MoreIndividual Mandate Tax – What is the Cost for Non-Compliance?
Last June the Supreme Court ruled that PPACA, including the individual mandate, is constitutional. Under the law, individuals are required to purchase health care insurance and if they do not, the penalty will be a tax. In order to avoid this tax, a person must have “minimum essential” coverage. This...
Read MoreHHS ISSUES PROPOSED RULES ON ‘BENEFIT AND PAYMENT PARAMETERS,’ MULTI-STATE PLAN PROGRAM
The following is a summary of proposed regulations. Some or all of the provisions may change when final rules are issued. On Dec. 5 and 7, 2012, the Department of Health and Human Services (HHS) issued two more sets of proposed rules that provide added details on how the Patient...
Read MoreHealth Care Reform Lunch N’Learns a Huge Success! More to come…
In light of the outcome of the November Presidential election, Innovative hosted three Lunch N’ Learn events over the last few weeks at Fleming’s Steak House in Marlton, DelFrisco’s Steak House in Philadelphia and Ruth’s Chris Steak House in Parsippany. We also joined Ultimate Software at a fourth event at...
Read MoreHIGHLIGHTS OF PROPOSED RULES ON HEALTH INSURANCE MARKET RULES
On Nov. 20, 2012, the Department of Health and Human Services (HHS) issued proposed rules that address a number of health insurance market reforms. The rule is still in the “proposed” stage, which means that there may — and likely will — be changes when the final rule is issued....
Read MoreHIGHLIGHTS OF PROPOSED RULES ON WELLNESS PROGRAMS
On Nov. 20, 2012, the Department of Health and Human Services, the IRS and the Department of Labor jointly issued a proposed rule that addresses how wellness programs may operate under PPACA beginning in 2014. The proposed rule would largely carry forward the rules that have been in effect for...
Read MoreHIGHLIGHTS OF PROPOSED RULES ON ESSENTIAL HEALTH BENEFITS AND ACTUARIAL VALUE
On Nov. 20, 2012, the Department of Health and Human Services (HHS) issued a proposed rule that addresses a number of questions surrounding essential health benefits and determining actuarial and minimum value. This rule is still in the “proposed” stage, which means that there may — and likely will —...
Read MoreHealthy Employees Lead to Wealthy Employees
We all know that employer-sponsored wellness programs are effective at extending quality of life by maintaining good health and reducing health risks that can worsen over time. Companies also obtain financials savings from implementing wellness programs. For instance, for every dollar spent on wellness, medical costs are reduced by $3.27...
Read MoreHealth Plan Design Drives Regional Costs
United Benefit Advisors (UBA), one of the nation’s largest employee benefit advisory organizations, announces more key findings from its 2012 Health Plan Survey. As health care costs continue to increase and recruitment and retention of quality employees becomes more competitive, accurate and detailed benefits benchmarking data is imperative for employee...
Read MoreWhat Employers Need To Know Right Now About Health Care Reform And What The Election Results Mean For PPACA
Maintenance of the status quo in Washington, D.C. (the re-election of Barack Obama, with a Republican majority in the House of Representatives and a Democratic majority in the Senate) means that implementation of the Patient Protection and Affordable Care Act (PPACA) will move forward largely as the law was passed...
Read MoreIn this Election, Health Care Takes Center Stage
By Thomas Mangan, CEO, United Benefit Advisors UBA and CFO magazine weigh in on the health insurance exchange market in the face of health care reform. Today marks a historic milestone in the leadership of America as millions of people head to the polls to elect or re-elect our president....
Read MorePlay or Pay: Applying the Employer Shared Responsibility Penalties
PPACA calls for two possible penalties, one for not offering “minimum essential” coverage and a different penalty for offering coverage that is considered inadequate because it is not “affordable” and/or it does not provide “minimum value.” (A) The “no offer” penalty applies if the large employer does not offer “minimum...
Read MorePlay or Pay: How Does an Employer Determine Average Hours Worked?
An employer may simply look at its population on a current, month by month basis if it wishes to. However, to avoid the complications that may arise if an employee alternates between working more and less than 30 hours, or to simply reduce calculation frequency, IRS Notice 2012-58 gives an...
Read MorePlay or Pay: How Will An Employer Count Hours?
It is expected that current DOL rules for counting hours for pension plan purposes will be used to count an employee’s hours of service as a full-time employee or full-time employee equivalent. Under these rules, a person is considered to have completed an “hour of service” with each hour for...
Read MoreCOMPLIANCE ALERT! CRITICAL AMENDMENT DEADLINE APPROACHING FOR DEFINED BENEFIT PLANS
Sponsors of single-employer defined benefit pension plans will need to amend those plans soon to comply with a critical requirement of the Pension Protection Act of 2006 (the PPA). As explained more fully below, meeting this deadline is crucial because the IRS has conditioned anti-cutback relief on a timely amendment. ...
Read MoreThe Play or Pay Penalty – How Are Employees Counted Under PPACA?
Determining how many employees you have is important for several purposes under the Patient Protection and Affordable Care Act (PPACA). So far, no final rules have been issued, but on Aug. 31, 2012, the regulatory agencies issued safe harbors for 2014 on several key issues. The agencies have also provided...
Read MoreImportant Information About New Jersey 51-100 Health Benefits Plans
A benefit feature that encourages use of generic drugs will be included in all 51-100 health benefits plans. All Aetna 51-100 new business and renewing plans with December 1, 2012 and later effective dates will include a benefit feature that encourages members to use generic drugs as a first choice....
Read MorePhiladelphia Interactive HR Workshop – “Strategies from Industry Leaders in an Era of Change”
Please join Innovative at the Ultimate Software interactive HR workshop. Innovative’s own Terriann Procida will be featured speaking about how to uncover the hidden risk in your benefit package through advanced analytics and predictive modeling. Your company needs a skilled and forward-thinking HR leader more than ever before. So are...
Read MoreUnited Benefit Advisors Welcomes Terriann Procida as a Board Member!
Terriann will be joining the United Benefit Advisors (UBA) Board of Directors effective January 1, 2013. As one of the nation’s largest employee benefits advisory organizations, UBA is comprised of more than 140 of the most successful and most trusted independent employee benefits advisory firms in North America and Europe. ...
Read MoreInnovative Speaks at MetLife Stadium!
Thank you Ultimate Software for inviting Innovative to be a part of your interactive HR workshop at MetLife Stadium yesterday in the Toyota Coaches Club! Our own Terriann Procida was asked to be a guest speaker at this fantastic event. Her presentation focused on changing the current reality of cost...
Read MoreNew Jersey Interactive HR Workshop
“Strategies from Industry Leaders in an Era of Change” Please join Innovative at the Ultimate Software interactive workshop. Innovative’s own Terriann Procida will be featured speaking about how to uncover the hidden risk in your benefit package through advanced analytics and predictive modeling. Your company needs a skilled and forward-thinking...
Read MoreMORE GUIDANCE ON “FULL-TIME” EMPLOYEES AND 90-DAY WAITING PERIOD
Starting in 2014, larger employers (generally, those with 50 or more employees) may face “shared responsibility” penalties if any of their “full-time” employees receive subsidized health coverage through an “Affordable Insurance Exchange.” At the same time, virtually all employer health plans will become subject to a 90-day limit on any...
Read MoreDo You Know What You Need To Know About Comparative Effectiveness Research Fees?
Under the Patient Protection and Affordable Care Act (PPACA), health insurers and self-funded plan sponsors will be required to pay a tax called the comparative effectiveness research fee. The proceeds are to be used to support research conducted by a Patient-Centered Outcomes Research Institute. This research will be centered on...
Read MoreIRS Issues Temporary Guidance for Identifying Full-Time Employees and Applying Waiting Periods
On Aug. 31, the IRS issued Notices 2012-58 and 2012-59, which provide safe harbors for 2014 (and perhaps beyond that date) on how to address some of the open questions on how the employer-shared responsibility penalties will apply. The notices affirm that employers that hire new employees who are reasonably...
Read MoreEmployers Prep for New Moves under PPACA
As the 2013 enrollment time draws near, employers are preparing to jump through a few extra hoops thanks to the recently reaffirmed health care reform law. In addition to the usual notices and benefit communications that employers must prepare and distribute to their employees, the Patient Protection and Affordable Care...
Read MorePPACA FSA Contribution Limits
• Applies to all employers who sponsor a health flexible spending account (FSA) • Effective as of the start of the 2013 plan year May not change plan year simply to delay application of the limit • Employee salary reduction contribution may not exceed $2,500 per health FSA per year...
Read MoreLEARN WHAT YOU NEED TO KNOW ABOUT PPACA
Nearly all employers will be affected by the Patient Protection and Affordable Care Act (PPACA) — but not necessarily in the same ways. A company’s compliance requirements largely will depend on its size, method of plan funding and other factors. Do you know which provisions apply to you? As a...
Read MoreHIGHLIGHTS OF W-2 REPORTING REQUIREMENT
• Must include the value of “employer-sponsored group health coverage” on W-2s beginning with the 2012 W-2 (to be issued in January 2013) • Except that, do not need to include this information if the employer issued fewer than 250 W-2s for the prior calendar year* o This means the...
Read MoreHIGHLIGHTS OF ADDITIONAL MEDICARE WITHHOLDING FOR HIGH EARNERS
• Effective Jan. 1, 2013 • Applies to all employers • Must withhold an additional 0.9 percent of the employee’s share for Medicare/HI (from 1.45 percent to 2.35 percent) once the employee’s wages exceed $200,000 Employer does not match this additional 0.9 percent Additional 0.9 percent is not capped Additional...
Read MoreMLR REBATE CONSIDERATIONS
Because the guidance provided by the regulatory agencies has been fairly general, employers continue to have questions about how to handle the medical loss ratio (MLR) checks. Below are answers to some common questions, based upon either the guidance issued by the agencies regarding MLRs or how similar situations have...
Read MoreHHS Report on MLR Provides Breakdown of Upcoming Rebates:
HHS has released a report on the first round of rebates to be provided under health care reform’s medical loss ratio (MLR) requirements. The report contains calendar year 2011 data–insurers are required to pay rebates by August 1, 2012 based on their 2011 MLR. The report provides a detailed breakdown...
Read MoreHealth Care Reform Still Stands – What Do Employers Need To Do Now?
On June 28th, the U.S. Supreme Court upheld the individual mandate and most of the Patient Protection and Affordable Care Act (PPACA). Because the individual mandate was found to be acceptable, most of the rest of the law (including the exchanges and the requirement that larger employers provide minimum coverage...
Read MoreOVERVIEW OF MEDICAL LOSS RATIO REBATES
The Affordable Care Act requires health insurers to spend a minimum percentage of their premium dollars on medical claims and quality improvement. Insurers in the large group market must achieve a medical loss ratio (MLR) of 85%, while insurers in the individual and small group markets must achieve an MLR...
Read MoreSUPREME COURT LARGELY UPHOLDS PPACA
Today, the U.S. Supreme Court upheld the individual mandate and most of the Patient Protection and Affordable Care Act (PPACA). As expected, it was a close decision — 5-4 — with Chief Justice Roberts and Justices Breyer, Ginsburg, Kagan and Sotomayor agreeing that the individual mandate is a permissible tax....
Read MoreCompliance Alert! PREPARING FOR THE SUPREME COURT DECISION ON HEALTH CARE REFORM
The U.S. Supreme Court is expected to publish its decision on the legality of the Patient Protection and Affordable Care Act, or PPACA (also called health care reform, HCR and ACA), by the end of June. What they will decide is anyone’s guess. Here are the possibilities (in no particular...
Read MoreTHE 2012 UBA HEALTH PLAN BENCHMARKING SURVEY HAS CLOSED AND THE WINNER OF THE NEW 32 GB IPAD IS…
THE WINNERS ARE: Herr Foods, Inc. and PREIT Services, LLC!!! Due to an overwhelming response to our 2012 UBA Health Plan Benchmarking Survey we are happy to announce that we have two winners for the New 32 GB iPad! With over 17,000 plans participating, including more than 100 plans from...
Read MoreHHS Releases Guidance on Exchanges, Including Draft Exchange Blueprint and Rules for Federally Facilitated Exchanges and SHOPs
HHS has issued a flurry of guidance on Exchanges, including a draft blueprint for use by states establishing an Exchange, and an outline of the agency’s approach to implementing a federally facilitated Exchange (FFE) and federally facilitated Small Business Health Options Program (FF-SHOP) in states that do not establish a...
Read MoreFinal Regulations Address Individual Tax Credit for Coverage Purchased Through Exchange
The IRS has published final regulations addressing various aspects of the premium tax credit enacted as part of health care reform. The final regulations address a number of technical issues affecting eligibility for and calculation of the tax credit. Here are some highlights of significance for employer-sponsored plans: • Guidance...
Read MoreThomas Mangan Joins UBA As New CEO
The UBA Board has selected Thomas Mangan, an insurance industry leader with more than 20 years of experience in the employee benefit marketplace, to serve as chief executive officer, effective immediately. As announced at UBA’s Spring Meeting earlier this week, Thom will take over the role and duties of Bill...
Read MoreInnovative Attends the 2012 Community Access Unlimited Golf Outing
Elizabeth, NJ – May 11, 2012 – While higher is not better on golf score cards the numbers turned in by the friends, supporters and community partners of Community Access Unlimited (CAU) at the agency’s 18th Annual Golf Classic were well above par. The May 10 event at Suburban Golf...
Read MoreNew Guidance on Summary of Benefits and Coverage Adds Safe Harbors
Starting on Sept. 23, 2012, health insurers and group health plans will be required to provide the summary of benefits and coverage (SBC) and the uniform glossary to consumers. On May 11, the Department of Labor’s Employee Benefits Security Administration, together with the Departments of Health and Human Services and...
Read MoreInnovative Exhibits at the 26th Annual Tri-State HRMA Conference
Innovative was once again thrilled to be a part of the Annual Tri-State HRMA Conference held at the Westin Hotel in Mount Laurel last Thursday. We enjoyed meeting all of the attendees while promoting our 2012 UBA Health Plan Benchmarking Survey. For anyone that started the survey there, they were...
Read MoreIRS ANNOUNCES 2013 AMOUNTS for HSAs and HDHPs
On April 27, the IRS issued Revenue Procedure 2012-26, announcing the 2013 inflation-adjusted dollar limitations applicable to health savings accounts (HSAs) and qualifying high-deductible health plans (HDHPs). The maximum HSA contribution for an individual with self-only coverage under an HDHP will increase to $3,250 – up from $3,100 in 2012. ...
Read MoreRevised Audit Guidelines
Recently, the Internal Revenue Service (IRS) published Revised Audit Guidelines for use by IRS auditors in examining group health plans for COBRA compliance. The revised Guidelines incorporate changes to account for laws that have affected COBRA since the previous guidelines were developed, such as the Health Insurance Portability and Accountability...
Read MoreState Exchange Regulations Issued
On March 12, the federal Department of Health and Human Services (HHS) released a revised version of the federal rules regarding the “Establishment of Exchanges and Qualified Health Plans and Exchange Standards for Employers.” Parts of the 644-page regulation have been issued as a final rule, meaning that they will...
Read MoreAgencies Issue Guidance on Waiting Periods
Under the ACA, effective for plan years beginning on or after January 1, 2014, a group health plan may not have a waiting period that exceeds 90 days. The ACA’s statutory language raised many questions regarding how this 90-day limit on waiting periods should be measured. Notice 2012-17 continues to...
Read MoreThe Innovative Award Goes To…
Innovative would like to congratulate UBA partner firm principal, Paul Bogumill of Mountain West Benefits in Helena, Montana, for receiving the Innovative Award at the annual Pharmacy Benefit Management Institute conference in Phoenix, Arizona. Paul was the brainchild behind the development of a new, innovative pharmacy benefit called URx. At...
Read MoreAgencies Issue Guidance on Employer Mandate
Employer Shared Responsibility A key element of the ACA is the employer “shared responsibility” provision. This provision, currently scheduled to take effect in 2014, would assess a penalty against certain “applicable large employers” (those with 50 or more full-time employees) that either fail to offer “minimum essential coverage” to their...
Read MoreAGENCIES ISSUE GUIDANCE ON AUTOMATIC ENROLLMENT
The ACA provision on automatic enrollment requires certain large employers (those with more than 200 full-time employees) to automatically enroll new full-time employees in one of the employer’s health benefit plans (subject to any legally permissible waiting period), and to continue the enrollment of current employees in a health benefit...
Read MoreThe Innovative Way!
Great job by Innovative’s Jeannine Bandiera, who found a way to make a member’s medication affordable! Recently one of our members was made aware of a tier change for the medication that she needs to treat her condition. The insurance carrier moved the medication to the Specialty Drug list from...
Read MoreHHS Releases Guidance Related to Annual Dollar Limit Waivers
On Feb. 13, 2012, the Department of Health and Human Services (HHS) stated a health insurance issuer that has received a waiver of the annual dollar limit requirements pursuant to Section 2711 of the Public Health Service Act for a group health insurance product can sell that product to a...
Read More2012 Fiscal Year Plans Must Adhere to FSA $2,500 Limit
Though not the norm, some Cafeteria Plans (Section 125 plans) are not calendar year plans but instead are fiscal year plans (e.g. February 1-January 31). Be careful if this applies to you because if your fiscal year plans include Health Care Spending Accounts (HCSA), then as the plan sponsor, you...
Read MoreIRS Releases 2011 Form 8941 and Instructions for Claiming
The IRS has released the 2011 version of Form 8941, which is used by eligible small employers to calculate their health care tax credit. Once calculated, the tax credit is claimed as a general business credit on Form 3800 (or by tax-exempt small employers as a refundable credit on Form...
Read MoreHHS Secretary Announces One-Year Delay for Nonprofits with Religious Beliefs in Complying with No-Cost Women’s Preventive Services
After receiving comments on the interim final rule requiring most health insurance plans to cover preventive services for women including recommended contraceptive services without copays, coinsurance or deductibles, Health and Human Services (HHS) Secretary Kathleen Sebelius announced that nonprofit employers who, based on religious beliefs, do not currently provide contraceptive...
Read MoreHHS Provides Illustrative Information Regarding Benchmarks for Essential Health Benefits
The Department of Health and Human Services (HHS) provided illustrative information to complement its Dec. 16, 2011, bulletin on essential health benefits (EHB) under the Patient Protection and Affordable Care Act. The information provides the names of the three largest products in the small group market in each state ranked...
Read MoreCategories
Archive







