New Jersey Pay Transparency Act Goes into Effect
As of June 1, 2025, New Jersey employers with 10 or more employees over 20 or more calendar weeks must comply with the New Jersey Pay and Benefit Transparency Act (“NJPBTA”). Covered employers include those doing business, employing individuals, or taking applications for employment within the state. What Does the Law Require?...
Read More
2024 EEO-1 Reporting Due June 24, 2025
The U.S. Equal Employment Opportunity Commission (EEOC) has announced that the 2024 EEO-1 Component 1 data collection deadline for employers to submit demographic data. For 2024, the filing platform opened May 20, 2025. Employers have until June 24, 2025, to submit their EEO-1 reports. The EEO-1 Component 1 report is a mandatory...
Read More
Federal Agencies Announce Pause on MHPAEA Final Rule Enforcement
The Consolidated Appropriations Act, 2021 (CAA) required medical plans to conduct a comparative analysis of the non-quantitative treatment limitations (NQTLs) under the plan. For the first few years following the enactment of the CAA, these rules were in a proposed state; however, in late 2024 the Department of Labor (DOL),...
Read More
IRS Issues 2026 HSA and EBHRA Limits
The IRS issued Revenue Procedure 2025-19, to announce the 2026 inflation-adjusted amounts for health savings accounts (HSAs), High-Deductible Health Plans (HDHPs) under the Internal Revenue Code (Code) and the maximum amount employers may contribute for excepted benefit health reimbursement arrangements (EBHRAs). The new HSA and HDHP limits will go into effect...
Read More
HHS Releases HIPAA Security Proposed Rules
In light of ongoing cybersecurity concerns related to HIPAA protected information and the Department of Labor’s guidance, which reiterated its focus on cybersecurity, the Department of Health and Human Services Office for Civil Rights (OCR) issued a notice of proposed rulemaking (NPRM) to the Security Rule under the Health Insurance...
Read More
RxDC Reporting Due June 1, 2025
The Centers for Medicare and Medicaid Services (CMS) has updated the Prescription Drug Data Collection (RxDC) resources. The updates include changes to the RxDC Reporting Instructions and new RxDC templates and data dictionary. As a reminder, the RxDC reporting was established as part of the transparency rules under the Consolidated Appropriations Act 2021...
Read More
Court Dismisses ERISA Fiduciary Class Action Against Johnson & Johnson
On January 24, 2025, the U.S. District Court of New Jersey dismissed two fiduciary breach claims in Lewandowski v. Johnson & Johnson, et al. (“Lewandowski”). In Lewandowski, the plaintiffs alleged Johnson & Johnson (“J&J”) breached its fiduciary duties to plan participants and beneficiaries by mismanaging its prescription drug plans when...
Read More
Medicare Part D Creditable Coverage Disclosure Due to CMS by March 1, 2025, for Calendar Year Plans
The Medicare Modernization Act (MMA) established annual notification requirements for employer-sponsored group health plans with prescription drug coverage. Per the MMA, employers sponsoring these plans are required to disclose annually the creditable status of the plan to The Centers for Medicare and Medicaid Services (CMS). This disclosure is due to...
Read More
National Philanthropy Day Award 2024
National Philanthropy Day was an amazing event put on by Association of Fundraising Professionals, New Jersey Chapter! Celebrating truly inspiring people in the heart of our South Jersey community! Innovative Benefit Planning was incredibly grateful to be recognized and joined by our community partners at the National Philanthropy Day Awards...
Read More
ACA Reporting Amendments Apply to Upcoming Reporting
President Biden signed two bills, Employer Reporting Improvement Act and the Paperwork Burden Reduction Act, into law which provide helpful updates to the Affordable Care Act’s (ACA) reporting requirements under Internal Revenue Code (IRC) Sections 6055 or 6056. The amendments are in effect for the 2024 reporting, which is due...
Read More
Updates for High Deductible Health Plans
Telehealth Flexibility Sunsetting in 2025 As a result of the CARES Act in 2020, HDHPs were permitted to provide first dollar telehealth coverage without negatively impacting HSA eligibility. This relief initially sunset in 2023. The Consolidated Appropriations Act, 2023 provided a two-year extension of the relief, with will not expire...
Read More
Secure 2.0 Retroactive Amendment
As we approach the end of the year, it’s important for Plan Sponsors to be aware of the new tax planning opportunities available under the SECURE Act. Plan Sponsors are now able to make a new tax-favored contribution to their existing plan after the close of their current tax year....
Read More
Deadline Approaching: HIPAA Rules to Limit the Use and Disclosure of PHI Related to Reproductive Health Care
As a result of the overturning of Roe v. Wade, the Department of Health and Human Services (HHS) released final rules aimed at ensuring the privacy of protected health information (PHI) related to lawful reproductive health care. Under the new rule, HIPAA-covered entities will be required to obtain signed attestation...
Read More
Gag Clause Prohibition Compliance Attestation Due by December 31, 2024
Background When the Consolidated Appropriations Act, 2021 (CAA) was enacted by Congress on December 27, 2020, the law included a provision preventing group health plans and health insurance carriers from entering into health plan services contracts (such as a third-party administrator or health care provider contracts) with gag clauses...
Read More
Delaware Paid Family and Medical Leave Opt-Out Deadline is Approaching
Overview of Delaware PFML: Starting January 1, 2026, Delaware’s PFML program will provide paid leave benefits to employees who have been employed for at least one year and have worked at least 1,250 hours in the most recent 12 months for various qualifying events, including: Caring for a new child...
Read More
Catch Up Provisions
New Catch-Up Limits Under Secure Act 2.0 As a plan sponsor, it’s crucial to stay informed about legislative changes that impact retirement plans. The Secure Act 2.0, signed into law on December 29, 2022, introduces several significant updates aimed at enhancing retirement security for Americans. One of the key optional...
Read More
MLR Rebates Due to Plan Sponsors by September 30, 2024
MLR Rebates Due to Plan Sponsors by September 30, 2024 The Affordable Care Act (ACA) outlines the requirements private health insurance issuers must follow, including obligations related to premium spending. The ACA requires health insurers to spend at least 80% to 85%, depending on the size of the market, of...
Read More
IRS Releases ACA Affordability Threshold for 2025
IRS Releases ACA Affordability Threshold for 2025 The IRS released Rev. Proc. 2024-25, announcing an increase in the ACA Affordability Contribution Rate from 8.39% in 2024 to 9.02% for the 2025 plan year. After three years of decreases in the ACA affordability threshold, this increase may be seen as welcome...
Read More
RetireReady NJ Exemption Registration is Fast Approaching!
RetireReady NJ Exemption Registration is Fast Approaching The New Jersey Secure Choice Savings Program Act requires certain New Jersey employers to establish a retirement savings program through the RetireReady NJ program, if they do not already sponsor a retirement savings plan. Once the program is established by the employer, New...
Read More
Court Issues Nationwide Block on the FTC’s Non-Compete Ban
The Court for the Northern District of Texas (the Court) issued a decision blocking the Federal Trade Commission’s (FTC) ban on non-compete agreements, which was set to go into effect September 4, 2024. The ban would have invalidated non-compete clauses, which typically prohibited workers from their previous employer’s competitor or...
Read More
Innovative’s Mark Sulpizio to speak at Garden State SHRM Conference
Learn more about the Garden State Council – SHRM Conference here! Secure Act 2.0 changes directly impact Roth accounts, IRA, 401(k), 403(b), and many related tax breaks; however, for the purposes of this document, the focus will be on 401(k) and 403(b) plans. Plan sponsors need to review their plan...
Read More
Upcoming Changes for HDHP Plan Sponsors Under Medicare Part D
Employers who sponsor group health plans must act now regarding the status of their prescription drug coverage in advance of changes to Medicare Part D that go into effect for 2025. The Inflation Reduction Act of 2022 (IRA) made changes to Medicare Part D to enhance benefits and enrollee cost...
Read More
Retirement Plan Checklist For Plan Sponsors
End of Year Checklist for Plan Sponsors: Ensuring Compliance and Maximizing Benefits As we approach the 4th quarter of 2024, it’s crucial for plan sponsors to take a proactive approach in reviewing their retirement plans. This end-of-year checklist will help ensure compliance with regulatory requirements and optimize the benefits for...
Read More
IRS Releases Education Assistance FAQs
The IRS recently released a Fact Sheet to address frequently asked questions related to educational assistance programs offered under IRC Section 127. Programs offered under this section allow employees to receive a tax-exempt benefit while providing employers with a tax deduction. The IRS noted that this Fact Sheet should not...
Read More
Secure 2.0 Student Loan Matching
The SECURE Act 2.0 allows employers to match employee student loan payments with retirement plan contributions. This benefit aims to help employees burdened with student debt save for retirement. Plan sponsors can implement this benefit to improve recruiting and retention. However, employers must navigate several considerations and challenges to implement...
Read More
Innovative Launches Secure 2.0 Act Readiness Checklist!
Secure Act 2.0 changes directly impact Roth accounts, IRA, 401(k), 403(b), and many related tax breaks; however, for the purposes of this document, the focus will be on 401(k) and 403(b) plans. Plan sponsors need to review their plan design, demographic data and discrimination testing to determine how the many...
Read More
Innovative Benefit Planning: 35 Years of Putting People First
This past February Innovative Benefit Planning was proudly featured in SJ Magazine for celebrating 35 years in business. We are grateful to have been recognized for our efforts, however, the true pride comes from the things we do for others, and the impact we make. Take a look at the article...
Read More
Innovative’s 5th Annual Well-Being @ Work Summit Recap
On May 7th, 2024 Innovative Benefit Planning hosted their 5th Annual Well-Being @ Work Summit, an event dedicated to making workplaces healthier, at the National Constitution Center in Philadelphia, PA! The morning started out on the right foot with breathwork and gentle stretching lead by Spencer Broad. Out on the...
Read More
Navigating Auto-Portability in Retirement Plans: Key Fiduciary and Liability Considerations Under SECURE Act 2.0
The introduction of auto-portability rules under SECURE Act 2.0 aims to simplify transferring small retirement accounts when employees change jobs, reducing cash-outs and enhancing retirement savings. However, plan sponsors must consider fiduciary and liability implications before adopting this feature. Fiduciary Responsibilities Plan sponsors are fiduciaries under the Employee Retirement Income...
Read More
PCORI Fee Due July 31, 2024
The Patient-Centered Outcomes Research Institute (PCORI) fee deadline is around the corner. In Notice 2023-70, the IRS adjusted the applicable dollar amount to be multiplied by the average number of covered lives for purposes of calculating the fee for policy years and plan years that end on or after October 1, 2023, and...
Read More
Secure 2.0 Auto-Portability
Auto-Portability Explained: Auto-portability is a feature designed to help plan participants consolidate their retirement accounts when they change jobs. Here’s how it works: Problem: When employees switch employers, they often leave behind small balances in their old 401(k) accounts. These “orphaned” accounts can lead to administrative burdens for plan sponsors and...
Read More
IRS Issues 2025 HSA and EBHRA Limits
The IRS issued Revenue Procedure 2024-25, to announce the 2025 inflation adjusted amounts for health savings accounts (HSAs), High Deductible Health Plans (HDHPs) under the Internal Revenue Code (Code) and the maximum amount employers may contribute for excepted benefit health reimbursement arrangements (EBHRAs). The new HSA and HDHP limits will go...
Read More
Secure 2.0 Involuntary Cash-Out Provision
In today’s complex benefits landscape, plan sponsors face the challenge of managing retirement plans efficiently while ensuring compliance and participant satisfaction. One effective solution is the practice of involuntary cash-outs, which involves automatically distributing the retirement accounts of former employees when balances fall below a specified threshold. Integrating this provision...
Read More
Johnson & Johnson Class Action Lawsuit
Johnson & Johnson Class Action Lawsuit In early February, a federal class action lawsuit was filed against Johnson & Johnson (JNJ) and its plan fiduciaries, alleging overpayment for prescription drugs within its prescription drug plan. The complaint alleges that under the Employee Retirement Income Security Act of 1974 (ERISA), JNJ’s...
Read More
SECURE 2.0: IRS Issues Guidance on De Minimis Financial Incentives and Employer Roth Contributions
The Secure Act 2.0 has been signed into law with the goal of promoting retirement security among Americans. The bill contains dozens of provisions that will impact various aspects of retirement plans. As a plan sponsor, it’s important to understand how the Secure Act 2.0 will impact your organization and...
Read More
Tax Planning Profit Sharing
Navigating the complexities of tax planning, employers are constantly on the lookout for strategies that not only maximize their financial health but also amplify the value they provide to their employees. Among these strategies, profit sharing emerges as a standout approach, marrying financial prudence with a commitment to employee welfare....
Read More
Civil Monetary Penalties Announced for 2024
Civil Monetary Penalties Announced for 2024 The Department of Labor (DOL) has announced the Civil Monetary Penalties for 2024. Federal agencies are required to review the penalty amounts annually to adjust for inflation, a requirement established in 2015 as part of the Federal Civil Penalties Inflation Adjustment Act Improvements Act....
Read More
Cyber-threat Reported by Change Healthcare and UnitedHealth Group
On February 21, 2024, Change Healthcare released information regarding a cybersecurity issue resulting in an enterprise-wide network interruption. Change Healthcare is part of the health services provider Optum, Inc., which is owned by UnitedHealth Group. By Thursday, February 22nd, both Change Healthcare and UnitedHealth acknowledged the issue and announced it...
Read More
Secure 2.0 Emergency Savings
The IRS recently issued guidance regarding various provisions of Secure Act 2.0, including the “Pension-linked Emergency Savings Account” (PLESA) provision. This provision aims to alleviate financial strain on employees facing hardships. Effective January 1st, 2024, non-highly compensated employees can contribute to an emergency savings account through payroll deferrals. Participants can...
Read More
RxDC Reporting due to CMS by June 1, 2024
The Centers for Medicare and Medicaid Services (CMS) has updated the Prescription Drug Data Collection (RxDC) resources. The updates include changes to the RxDC Reporting Instructions and new RxDC templates and data dictionary. As a reminder, the RxDC reporting was established as part of the transparency rules under the Consolidated...
Read More
New Employee Classification Rule
In January, the Department of Labor (DOL) Wage and Hour Division introduced a rule that changes the way workers are classified under the Fair Labor Standards Act (FLSA). This Final Rule, effective March 11, 2024, offers a more comprehensive test to determine a worker’s status, potentially making it more challenging...
Read More
Medicare Creditable Coverage Disclosure Due to CMS by March 1, 2024
The Medicare Modernization Act (MMA) established annual notification requirements for employer-sponsored group health plans with prescription drug coverage. Per the MMA, employers sponsoring these plans are required to disclose annually the creditable status of the plan to The Centers for Medicare and Medicaid Services (CMS). This disclosure is due to...
Read More
Guidance On Coverage For Contraceptives
The Affordable Care Act (ACA) Implementation FAQs Part 64, issued on January 22, 2024, provide guidance on preventive service coverage. Prepared by the Departments of Labor, Health and Human Services, and the Treasury, they aim to enhance understanding and compliance with the law and specify that non-grandfathered health plans must...
Read More
2024 ACA Reporting Code Reference Sheet
2024_ACAReportingCodesReference 2024_ACAReportingCodesReference
Read More
IRS Issues Additional Guidance for SECURE 2.0 Act
In an effort to provide necessary clarity for employers and plan sponsors, the Internal Revenue Service (IRS) issued long-awaited guidance for various provisions under the SECURE 2.0 Act (SECURE 2.0). This guidance comes in Question-and-Answer format and addresses twelve of the 90+ provisions under SECURE 2.0. Specifically, provisions related to...
Read More
IRS Releases 401(k) Guidance For Long-Term Part-Time Employees Under the Secure 2.0 Act
On November 24, 2023, the IRS released long-awaited guidance around the updated 401(k) eligibility requirements pertaining to long-term part-time employees (LTPT) under the SECURE 2.0 Act of 2022 (SECURE 2.0). These proposed regulations, if finalized, would amend the rules previously applicable to 401(k) plans and provide additional clarification for some...
Read More
IRS Issues 2024 FSA and Commuter Limits
On November 9, 2023, the IRS released the long awaited 2024 maximum contribution limits for Flexible Spending Arrangements (FSA) and Commuter accounts. A bit later than usual, Revenue Procedure 2023-34 follows the IRS’s announcement of the 2024 401(k) annual contribution limits, which were released November 1st. For taxable years...
Read MorePS Plan and Retroactive Amendment
Under the SECURE Act, employers can adopt a profit-sharing plan for the prior year, as long as the plan is established before the employer’s tax-filing deadline, including extensions. This means that an employer could potentially adopt a profit-sharing plan as late as October 15th of the following year. Effective on...
Read More
Departments Move Forward with Enforcement of Deferred Machine-Readable File Requirement
The Departments of Labor, Health and Human Services and Treasury (The Departments) have released updated FAQs around the requirement for plans and issuers to post machine-readable files on a public website. Per the Consolidated Appropriations Act, 2021 (CAA), plans and issuers were required to post, in three separate machine-readable files,...
Read More
Joint Agency Guidance on Gag Clause Prohibition for Health Plan Agreement
On February 23, 2023, the Department of Labor (DOL), the Department of Health and Human Services (HHS), and the Internal Revenue Service (IRS) (the “Agencies”) released FAQs addressing the implementation of certain transparency requirements under the Consolidated Appropriations Act of 2021 (CAA). These joint-issued FAQs address additional compliance guidance on...
Read More
Ways to Improve Retirement Planning
As a plan sponsor, enhancing retirement plan performance is vital for the benefit of both participants and the plan’s long-term success. Effective strategies to improve retirement plan performance include: Implementing automatic features, such as enrollment and deferral escalation Offering a diverse menu of investment options for participants of all investment...
Read More
IRS Delays Roth Catch-Up Contribution Requirement under SECURE 2.0 Act
In light of concerns expressed by plan sponsors and participants alike, the IRS released Notice 2023-62 (“Notice”) which provides a two-year extension on the requirement related to Roth catch-up contributions under SECURE 2.0 Act (“the Act”). Specifically, the Notice states, “The Department of Treasury and the IRS have been made...
Read More
EEOC Announces 2022 EEO-1 Component 1 Submission Deadline
The U.S. Equal Employment Opportunity Commission (EEOC) has announced that the 2022 EEO-1 Component 1 data collection deadline for employers to submit demographic data. For 2022, data collection will begin on October 31, 2023. Eligible employers have until December 5, 2023, to submit their EEO-1 reports. The EEO-1 Component 1...
Read More
IRS Releases ACA Affordability Threshold for 2024
The IRS released Rev. Proc. 2023-29on August 23, 2023, announcing a decrease in the ACA Affordability Contribution Rate from 9.12% in 2022 to 8.39% for the 2024 plan year. This is an even greater decrease from what was announced for the 2023 tax year, which was formerly the most significant...
Read More
Notice of Proposed Rulemaking Released for the Pregnant Workers Fairness Act
The U.S. Equal Employment Opportunity Commission (EEOC) has issued a Notice of Proposed Rulemaking around the implementation of the Pregnant Workers Fairness Act (PWFA). The proposed rule, released for inspection August 7, 2023, aims to provide some needed clarification for employees and employers as they navigate the requirements under PWFA....
Read MoreFee Transparency
Fee analysis and transparency are vital for successful retirement plans. Understanding fee impacts and conducting benchmarking helps plan sponsors make informed decisions and protect themselves as fiduciaries. Below, we explore various fee types, and offer guidance for effective fee management in retirement plans. Fee analysis affects plan performance directly. Transparent...
Read More
New FAQ On No Surprise Act
Recently, the Departments of Labor, Treasury, and Health and Human Services (the “Departments”) released new frequently asked questions (FAQs) on the No Surprises Act and the Transparency in Coverage final rules, giving employers more guidance and clarity around health plan out-of-network providers and fee disclosures. Under the Affordable Care Act...
Read MoreFlu Season is Approaching
Flu Season is Approaching – Let Innovative Workplace Wellness arrange a flu shot clinic for your employees. Flu season is quickly approaching and the best way to protect yourself and your employees from the flu is to get a flu shot. Reducing the spread of respiratory illnesses, like the flu,...
Read More
MHPAEA Opt-Out Expires
The Centers for Medicare & Medicaid Services (CMS) has issued guidelines regarding changes to the Mental Health Parity and Addiction Equity Act (MHPAEA) for self-insured non-federal governmental health plans. The Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) requires group health plans and health insurance issuers to ensure...
Read More
IRS Issues Guidance Related to Taxability of Wellness Indemnity Plan Payments
The IRS issued its fourth Chief Counsel Advice 202323006 (the “CCA”) to address the tax treatment of payments made to employees through employer-funded fixed indemnity insurance policies. Specifically, the guidance speaks to how wellness indemnity payments should be treated in the event an employee has unreimbursed out-of-pocket medical expenses related...
Read More
DHS Terminates I-9 Form Remote Option Flexibility; Considerations for Remote Workers
For employers that remotely verified I-9 forms during the pandemic, the deadline for completing in-person verification is fast approaching. As background, the Department of Homeland Security (DHS) had provided additional flexibility due to COVID-19 to review I-9 documentation remotely and had previously announced that employers would have until July 31,...
Read More
Pregnant Workers Fairness Act Goes Into Effect
Part of the Consolidated Appropriations Act, 2022, effective June 27, 2023, the Pregnant Workers Fairness Act (PWFA) requires employers with 15 or more employees to provide reasonable accommodations for job applicants and employees with known limitations related to pregnancy, childbirth and related medical conditions. The PWFA covers only accommodations and does not...
Read More
Participant Retirement Readiness
Assessing the effectiveness of your retirement plan is vital for ensuring participants’ readiness for retirement. By measuring retirement readiness, evaluating your plan’s performance, and implementing key strategies, you can improve participants’ preparedness. In this blog, we will discuss the importance of measuring retirement readiness, provide insights into evaluating plan effectiveness,...
Read More
PCORI Fee Due July 31, 2023
The Patient-Centered Outcomes Research Institute (PCORI) fee deadline is around the corner. In Notice 2022-59, the IRS adjusted the applicable dollar amount to be multiplied by the average number of covered lives for purposes of calculating the fee for policy years and plan years that end on or after October 1, 2022, and...
Read More
IRS Issues 2024 HSA and EBHRA Limits
The IRS issued Revenue Procedure 2023-23, to announce the 2024 inflation adjusted amounts for health savings accounts (HSAs), High Deductible Health Plans (HDHPs) under the Internal Revenue Code (Code) and the maximum amount employers may contribute for excepted benefit health reimbursement arrangements (EBHRAs). Significant increases to the limits are a...
Read More
5 Reasons to Hire a Financial Advisor for Your Retirement Plan
When managing a retirement plan, plan sponsors are faced with decisions that can affect the entire organization such as plan design, investment line-up, and who the recordkeeper will be. Unfortunately, many plan sponsors are not experts in qualified retirement plans or the ERISA laws that govern them. Decision makers for...
Read More
Federal Appeals Court Issues Stay On ACA Judgement
The Fifth Circuit Court of Appeals has issued a stay on a lower court ruling striking down certain preventive care coverage mandates under the Affordable Care Act. On March 30, 2023, the U.S. District Court in the Northern District of Texas issued its final ruling invalidating provisions of the ACA’s...
Read More
Missing Participant and Uncashed Checks
As a plan sponsor of a company retirement plan, it is important to have a process for locating missing participants and notifying participants of uncashed checks. Failure to do so can result in penalties and fines from regulatory agencies, as well as potential litigation from participants. Missing participants are those...
Read More
Federal Judge in Texas Strikes Down Key ACA Provision Regarding Preventive Care Services
On March 30, 2023, the U.S. District Court in the Northern District of Texas (Court) issued a final ruling invalidating certain provisions of the Affordable Care Act’s (ACA) preventive care mandate. Although the ultimate outcome of this decision remains to be seen, the ruling has created some confusion for plan...
Read More
DOL Signals July 10 as End of COVID-19 Outbreak Period, Despite Early End to National Emergency
On Monday, April 10, 2023, President Biden signed Congress’s jointly-introduced H.J Res. 7 into law, ending the COVID-19 National Emergency immediately instead of on May 11, 2023, as previously announced. However, the Department of Labor (DOL) has unofficially signaled that its previous guidance issued on March 29, 2023, stands, including...
Read More
Temporary Workers’ Bill of Rights Signed into Law in New Jersey
In early February 2023, Governor Phil Murphy signed the Temporary Workers’ Bill of Rights (the Bill) which expands the rights and protections afforded to temporary workers. The Bill is applicable to temporary laborers in a “designated classification placement,” which is defined as an assignment of a temporary laborer by a...
Read More
Profit Sharing Plan and Retroactive Amendment
As a follow-up to last month’s blog on the benefits of retroactively establishing a profit-sharing plan, the Secure Act 2.0 also gives retirement plan sponsors the ability to retroactively amend their existing plans to increase plan benefits as long as the plan is amended prior to the filing of the...
Read More
President Biden Adopts the New Regulations Impacting Working Mothers
Congress recently passed, through the Consolidated Appropriations Act, 2023, the PUMP for Nursing Mothers Act (the Act) which makes several changes to the Break Time for Nursing Mothers law, enacted in 2010. Under the Break Time for Nursing Mothers law, employers nationwide were required to provide reasonable break time and...
Read More
Internal Revenue Service Releases 2024 ACA Penalty Amounts
The Internal Revenue Service (IRS) released Rev. Proc. 2023-17, which outlines the inflation adjustments for the employer shared responsibility payments (ESRP) under the Affordable Care Act (ACA). Under the ACA’s pay or play rules, applicable large employees (ALEs) must offer affordable minimum-value health coverage to their full-time employees or be...
Read More
Tax Planning and Profit Sharing Plan
If you’re a business owner looking to save for retirement while also reducing your taxable income, adding a profit-sharing component to an employer retirement plan could be an attractive option. Not only does it allow you to set aside a portion of your profits for your retirement, but a profit-sharing...
Read More
President Biden Reveals Plan to End National COVID-19 Emergency
On January 30 President Biden issued a statement of policy to Congress in which he announced that the administration plans to end both the National Emergency related to COVID-19 originally declared by President Trump in 2020 and the public health emergency (PHE) declared by the U.S. Department of Health and...
Read More
EEOC Updates Guidance Related to COVID-19 Workplace Testing
In recognition of the changing circumstances related to the COVID-19 pandemic, the EEOC has updated its guidance around conducting testing for on-site employees. Employers covered by the Americans with Disabilities Act must assess whether the current workplace circumstances within their organization justify COVID-19 testing, if they are continuing to test....
Read More
Biden Administration Enacts Speak Out Act
Ahead of the close of the 117th U.S. Congress, the House of Representatives, with a vote of 315 – 109, quietly passed the Speak Out Act (“The Act”). President Biden signed the bill a few weeks later. Under the new law, nondisclosure and non-disparagement clauses related to allegations of sexual...
Read More
Feds Extend Prescription Drug Filing Deadline, Announce Relaxed Enforcement
The Departments of Labor, Health and Human Services, and the Treasury (collectively, the Departments) last week issued an FAQ that relieved filing entities from the December 27, 2022, deadline for providing certain information. The Departments understood many plans and carriers faced significant operational challenges in complying with the reporting requirements,...
Read More
Continuing Appropriations Act Extends HDHP Relief for Telehealth Services
President Biden last week signed the Continuing Appropriations Act, 2023 (CAA 23) to provide funding for the federal government through the current fiscal year. But employers also should know there were some critical benefits-related provisions tucked into CAA 23. Though many of the benefits sections of CAA 23 related to...
Read More
Innovative Named A Samaritan Gala Honoree
Innovative Benefit Planning is honored to be recognized as a “2023 Celebration of Life Gala Honoree” at this year’s Samaritan Gala. Each year, Samaritan honors an individual and/or company for their continued passion, dedication, and love for Samaritan and the community. This year, Samaritan is recognizing Innovative for our commitment...
Read More
Secure Act 2.0
The Secure Act 2.0 is poised to be signed into law with the goal of promoting retirement security among Americans. The bill contains dozens of provisions that will impact various aspects of retirement plans. As a plan sponsor, it’s helpful to understand how the Secure Act 2.0 will impact your...
Read More
Employers Prepare For Rx Reporting Deadline
Section 204 of the 2021 Consolidated Appropriations Act (CAA) outlined several requirements for group health plans and health insurers aimed at targeting rising prescription drug costs. In an effort to bolster transparency, the CAA created new obligations for plans to report specific prescription drug data to The Centers for Medicare...
Read More
Cafeteria Plans: Change in Status Events and Permissible Employee Election Changes
Cafeteria plans are governed by IRS Code Section 125 and allow employers to help employees pay for expenses such as health insurance with pre-tax dollars. Employees can choose between a taxable benefit (such as cash) and two or more specified pre-tax qualified benefits (health insurance, for example). Employees can select...
Read More
Updated: Temporary Flexibilities for Remote Document Examination for Form 1-9 Extended
Temporary Flexibilities for Remote Document Examination for Form I-9 Extended Again In March 2020, the Department of Homeland Security (DHS) and U.S. Immigration and Customs Enforcement (ICE) instituted a temporary policy which allowed employers with a remote workforce to defer physical presence requirements associated with Form I-9 and Section 274A...
Read More
“Family Glitch” Final Rule Released
Published October 13, 2022, The Department of Treasury released finalized regulations that make the premium tax credit (PTC) for Marketplace health coverage available to more individuals starting in 2023. Under the Affordable Care Act (ACA) regulations, employer-based health insurance is deemed “affordable” if the employee’s contribution for self-only coverage does...
Read More
Substantial Medical Loss Ratio Rebates Expected in 2022
Per the Kaiser Family Foundation, an estimated 8.2 million Americans will be due rebates for 2022. Further the analysis states that health insurers are expected to pay a total of $1 billion to policyholders. In light of this, plan sponsors should be prepared to handle any Medical Loss Ratio (MLR)...
Read More
Health Plan Disclosure Requirements for Prescription Drugs
Under the Affordable Care Act (ACA) transparency-in-coverage (TiC) rules and provisions of the Consolidated Appropriations Act, 2021 (CAA), group health plan sponsors must both disclose and report detailed information regarding a plan’s prescription drug coverage and costs. There is significant overlap under the two sets of disclosure rules, which has...
Read More
Departments Issue No Surprises Act FAQ and Clarify Independent Dispute Resolution Process
The U.S. Departments of Health and Human Services, Labor, and the Treasury (the “Departments”) recently released final rules regarding the No Surprises Act. The rules specifically address required independent dispute resolution (IDR) of certain claims and expenses and finalize prior interim final rules relating to information that group health plans...
Read More
Innovative Benefit Planning Receives Women’s Business Enterprise Owned Certification
Innovative Benefit Planning is proud to announce that The Women’s Business Enterprise National Council, has awarded Innovative Benefit Planning the national ‘Women’s Business Enterprise’ certification. “Empowering women in the workplace and acknowledging their contributions to everyday operations is not only important but extremely necessary,” said Terriann Procida, CEO. “Having a...
Read More
President Biden Signs Inflation Reduction Act Into Law
On August 16, 2022, President Biden signed the long-awaited Inflation Reduction Act which aims to reduce rising health care costs and greenhouse gas emissions, as well as raise taxes on corporations. The President’s signature comes after the House and Senate passed the bill last week along party lines following much...
Read More
Biden Administration’s Fiscal Year 2023 Budget Calls for Increased Enforcement for MHPAEA
The Biden Administration’s FY 2023 proposed budget requests increased funds to enforce the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA). Specifically, the budget would allot $125 million to the states for MHPAEA enforcement. Additionally, President Biden requested an additional $275 million for the Department of Labor (DOL)...
Read More
FDA Issues Final Rule Enabling Access to Over-the-Counter Hearing Aids
Around 30 million adults in the U.S. deal with some form of hearing loss, but only an estimated 1 in 5 have addressed the issue with the use of a hearing assistance device. On August 16, 2022, the U.S. Food and Drug Administration (FDA) issued a final rule that would...
Read More
IRS Announces ACA Affordability Contribution Percentage for 2023
The IRS announced a decrease in the ACA Affordability Contribution Rate from 9.61 in 2022 to 9.12 percent for the 2023 plan year, the most significant decrease since the ACA’s commencement. Under the ACA, Applicable Large Employers (ALEs), employers with 50 or more full time and/or full-time equivalent employees, are...
Read More
June/July 2022 Compliance Recap
The summer has seen a flurry of compliance-related activity, most notably the landmark decision issued by the U.S. Supreme Court to overturn Roe v. Wade. As we move into the second half of the 2022 employee benefits compliance calendar, there are a number of important issues to note. SCOTUS OVERTURNS ROE...
Read More
HHS Issues Proposed Rules under ACA Section 1557 to Clarify Scope of Discrimination Protections
The U.S. Department of Health and Human Services (HHS) has announced a proposed rule (Proposed Rule) implementing Section 1557 of the Affordable Care Act (ACA) that prohibits discrimination on the basis of race, color, national origin, sex, age, and disability in certain health programs and activities. The Proposed Rule is...
Read More
Retirement Plan Solutions to Address the Tight Labor Market
Employers who face staffing challenges in the current worker-driven labor market are implementing innovative retirement plan solutions to help them recruit new candidates and retain experienced personnel. Over the past two years, organizations have lost millions of valued team members as the Great Resignation and the Great Retirement boosted turnover....
Read More
Transparency in Coverage: Machine Readable Files
July 1, 2022, marks the effective date for plans and issuers to begin posting two Machine-Readable Files (MRF) links to a public website so individuals can readily learn their in-network group health plan costs, as well as historical paid amounts for out-of-network services. Ahead of this deadline, plans and issuers...
Read More
Innovative Benefit Planning Named “Top Employee Benefits Consultant” Award
Innovative Benefit Planning is honored to be recognized by Mployer Advisor as a winner of their “Top Employee Benefits Consultants” Awards for 2022. The program evaluates brokers based on breadth and depth of experience across employer industries, sizes, insurance products, and employer reviews. Innovative was recognized as a broker that...
Read More
Supreme Court Issues Ruling in Dialysis Case
In a 7-2 decision, the U.S. Supreme Court has issued its opinion in Marietta Memorial Hospital Employee Health Benefit Plan v. DaVita Inc., ruling in favor of Marietta Memorial Hospital’s health plan. In the Court’s opinion, drafted by Justice Brett Kavanaugh, the Court held the plan did not violate a...
Read More
An Employer’s Guide to Workplace Protections for Abortion-Related Decisions
Employers likely have questions about abortion-related employment protections and healthcare benefits after Friday’s SCOTUS controversial decision that overturned Roe v. Wade. Given the ruling, people in states with strict abortion limitations may end up traveling to other states to receive abortion-related care. Can employees take job-protected leave to obtain such...
Read More
Innovative Launches Employee Lifecycle Tool Kit
Innovative is excited to launch our Employee Life Cycle Tool Kit! Today’s tight labor market and the broad range of flexible work/life options make it more important than ever to properly manage each step in the employee lifecycle. Addressing their emerging needs means employers must engage their teams at each...
Read More
7 Low-Cost Initiatives Employers Can Incorporate in Their D&I Programs Now
Countless studies show that employers who focus on diversity and inclusion policies and practices help increase employee engagement and boost overall happiness in the workplace, thus improving retention. Research shows that companies with diverse, inclusive teams generate 19% more revenue and perform 35% better than their industry average. While integrating...
Read More
May 2022 Compliance Recap
The month of May again brought relatively little major employee benefit compliance guidance from federal agencies. However, there was plenty of activity in the courts to provide useful insight into steps employer plan sponsors can take to safeguard against benefits litigation. DEPARTMENT OF LABOR PROVIDES MENTAL HEALTH CONDITION GUIDANCE UNDER...
Read More
What Health Plan Sponsors Need to Know about Publishing Machine-Readable Files
June 1, 2022 As of July 1, 2022, group health plans must clear one of the first major compliance hurdles required by the Affordable Care Act’s (ACA) Transparency in Coverage (TiC) Final Rules. By that date, plans and insurance carriers must have prepared and posted two machine-readable files (MRFs) to...
Read More
Temporary Flexibilities for Remote Document Examination for Form I-9 Extended
In March 2020, the Department of Homeland Security (DHS) and U.S. Immigration and Customs Enforcement (ICE) instituted a temporary policy which allowed employers with a remote workforce to defer physical presence requirements associated with Form I-9 and Section 274A of the Immigration and Nationality Act. Initially applicable only to employers...
Read More
April 2022 Compliance Recap
After several very quiet months this year, April saw renewed compliance activity. The IRS provided guidance on transportation fringe benefits unused due to COVID-19 workplace changes and announced inflation-adjusted amounts for HSAs and HRAs. The Centers for Medicare & Medicaid Services (CMS) announced Medicare Part D rates and the parameters...
Read More
Innovative’s 3rd Annual Well-Being @ Work Summit Recap
On May 12th, 2022 Innovative Benefit Planning hosted the 3rd Annual Well-Being @ Work Summit, an event dedicated to making workplaces healthier, at the Adventure Aquarium in Camden, NJ! The morning started out on the right foot with complimentary biometric screenings and breakfast during registration, while attendees also had time...
Read More
2022 Patient-Centered Outcomes Research Institute (PCORI) Fee
The Patient-Centered Outcomes Research Institute (PCORI) fee deadline is around the corner. In Notice 2022-4, the IRS adjusted the applicable dollar amount to be multiplied by the average number of covered lives for purposes of calculating the fee for policy years and plan years that end on or after October 1, 2021,...
Read More
Innovative Gets Certified in Mental Health First Aid Training in the Workplace
Innovative Benefits Planning is pleased to announce that our Nurse Advocate, Erica Polaneczky, has become certified in Mental Health First Aid Training. This certification allows her to provide Mental Health First Aid in the workplace training for employers. Mental Health First Aid (MHFA) teaches employers how to identify, understand, and...
Read More
IRS Issues 2023 HSA and HRA Limits
The IRS issued Revenue Procedure 2022-24, to announce the 2023 inflation adjusted amounts for health savings accounts (HSAs) under Section 223 of the Internal Revenue Code (Code) and the maximum amount employers may contribute for excepted benefit health reimbursement arrangements (HRAs). Significant increases to the limits are a result of the...
Read More
Utilizing Pulse Surveys and Stay Interviews for Retention and Culture
Keeping your employees engaged in their work is an ongoing component in the employee life cycle. This directly leads to their retention and success in the organization. Retaining your employees and how that impacts overall culture are important to stay on top of. For many organizations, conducting exit interviews has...
Read More
37% of Employees Cite Stress for Leaving Their Job: Learn How You Can Prevent This
Employers who are already challenged to find and keep top talent amidst a tough job market may find that high levels of workplace stress are making it more difficult to assemble and sustain a solid workforce. Recruiting and Retention With stress levels higher than ever in the early 2020s, several...
Read More
Innovative is Featured in SJ Magazine for Creating a Culture of Giving Back
Innovative Benefit Planning LLC was proudly featured this month in SJ Magazine for our culture of “giving back” to our community. We are grateful to have been recognized for our efforts, however the true pride comes from the things we do for others, and the impact we make. Take a...
Read More
2021 EEO-1 Component 1 Data Collection Portal is Now Open
The U.S. Equal Employment Opportunity Commission (EEOC) has announced that the 2021 EEO-1 Component 1 data collection portal is now open. Eligible employers have until May 17, 2022, to submit data to the portal. The EEO-1 Component 1 report is a mandatory annual data collection that requires all private sector...
Read More
Are You Leveraging Population Health Management Correctly to Mitigate Claims Risk?
While all health plans face the possibility of higher claims, properly managing your employee’s risk pool and population health can help mitigate claims risk and reduce costs in your plan. Population health management identifies, evaluates, and manages the risks facing an organization and its plan participants. While employers cannot prevent...
Read More
Three Major Differences Between a Broker and Fiduciary Plan Sponsor
For plan sponsors, managing a 401(k) plan can be complex and time-consuming. Some plan sponsors hire outside advisors to help the plan stay compliant with the various IRS and ERISA regulations. When hiring outside advisors, many plan sponsors are unaware of the added benefits of hiring an investment fiduciary as...
Read More
9 Things to Consider About Your Advance Directive
It is no surprise that Stress Awareness Month and National Healthcare Decisions Day fall on the calendar simultaneously. If you are caring for a parent, spouse, or other family member, you want to honor their wishes, values, and goals. At the same time, you are no stranger to the stress...
Read More
Proposed Rule Would Fix the “Family Glitch”
Under the current Affordable Care Act (ACA) regulations, employer-based health insurance is deemed “affordable” if the employee’s contribution for self-only coverage does not exceed the affordability threshold in a given year (9.61% in 2022). Those who do not have access to affordable employer-based coverage may qualify for a premium tax...
Read More
House Passes Secure Act 2.0 Bill
In a 414-5 bipartisan vote, the House of Representatives has passed a bill that, if enacted, is said to improve the retirement savings system in the United States by expanding coverage and increasing retirement savings. The Securing a Strong Retirement Act, colloquially known as Secure Act 2.0 builds on the...
Read More
Temporary Flexibilities for Expired List B Identity Documents to End
In May 2020, the Department of Homeland Security (DHS) instituted a temporary policy which allowed employees to present expired List B identification documents for I-9 purposes. As a reminder, Form I-9 is used to verify the identity and employment authorization of individuals hired for employment in the United States. This...
Read More
Innovative Announces the 3rd Annual Well-Being @ Work Summit
Innovative is excited to announce the date for our 3rd annual Well-Being at Work Summit. Join us on Thursday, May 12th, from 9:00am-3:00pm, at Adventure Aquarium in Camden, New Jersey. This Year’s Theme: Unfortunately, due to things like the pandemic, isolation and burnout, employee mental illness is on the rise....
Read More
Government Funding Bill Extends CARES Act Relief for HDHPs
President Biden recently signed The Consolidated Appropriations Act, 2022 (CAA) into law. As part of the 2022 CAA, COVID-related telehealth coverage can be covered at no cost-share for High Deductible Health Plans (HDHPs) in a similar fashion to what was allowed under the CARES Act starting April 1, 2022 through...
Read More
The DOL’s Compliance Assistance Release No. 2022-01 401(k) Plan Investments in “Cryptocurrencies”
As plan advisors, we’ve had increasing questions from plan sponsors and committees about the availability and merits of Crypto backed investment options. With their release last week, the DOL has made their position very clear: they will investigate plan fiduciaries who make these types of investments available, even through brokerage...
Read More
Tax Planning Opportunities Through Proper Retirement Plan Design
Many business owners, principals, and executives are not aware of the tremendous personal and corporate tax benefits that can be achieved through the proper retirement plan design. Most retirement plans are designed for administrative efficiency – not for tax planning purposes. As a result, most businesses are not aware of...
Read More
Four Steps to Create a Stable Renewal Environment
Large renewal rate increases frustrate employers and plan sponsors each year. They might experience significant, double-digit rate hikes one year; a smaller uptick the second; and another large increase the third year. Owners, CFOs, and HR executives would prefer stable, predictable trends so they can better budget for future costs....
Read More
The Connection of Healthy Hearts and Minds in the Workplace
American Heart Month, observed every February since 1963, raises awareness about the dangers of heart disease and promotes lifestyle changes that can help people improve their heart health. Despite this, heart disease remains the leading cause of death among Americans. However, the American Heart Association (AHA) is now expanding the...
Read More
January 2022 Compliance Recap
January brought breaking news that the U.S. Supreme Court (the Court) would stop OSHA from enforcing its employee COVID-19 test or vaccinate emergency temporary standard (ETS) for employers with 100 or more employees. Although the decision doesn’t end the OSHA ETS permanently, it means that the ETS is unlikely to...
Read More
Departments Clarify Required Coverage of At-Home OTC COVID-19 Tests
The Departments of Labor, Health and Human Services, and the Treasury (collectively, the Departments) recently issued updated FAQ guidance to explain how employer group health plans may comply with the requirement to cover with no cost-sharing or preauthorization at-home over-the-counter (OTC) COVID-19 tests provided with no prescription or health care...
Read More
Delivery Requirements for Summary Plan Description
It’s so important for employers to understand the requirements around annual notices and annual delivery of theirs SPDs and their SBCs. There is great potential for a penalty if an employee were to request that document and not receive it within 30 days; those penalties can be up to $100...
Read More
How to Reset & Reflect After Benefits Renewal Season
The hectic benefits renewal season is finally winding down for many employers, with open enrollment meetings and all the logistical challenges and decisions behind us for 2021. We’re ready to relax and move on to new challenges during the new year. But wait a second: maybe we shouldn’t put renewal season...
Read More
Solutions for Recruiting in a Candidate-Driven Market
Employers recruiting top-quality talent face new challenges as they navigate the current candidate-driven market. During 2020, the pandemic gave us an employer-driven market, where high unemployment rates and reducing hiring meant more candidates competed for fewer openings. By mid-2021, the dynamic shifted to a candidate driven-market, as the economic recovery...
Read More
Government Distribution of Free at-home COVID-19 tests
Starting January 19th, 2022, Americans will be able to order a test online at COVIDTests.gov. To ensure broad access, the program will limit the number of tests sent to each residential address to four tests. Tests will usually ship within 7-12 days of ordering. To help distribute the message to...
Read More
Supreme Court Blocks OSHA Vaccine-or-Test Mandate But Allows Vaccine Mandate for Healthcare Workers to Proceed
Oral arguments on the OSHA vaccine-or-test mandate and vaccine mandate for healthcare workers were heard on January 7, 2022. As a result, the U.S. Supreme Court has issued two opinions with different outcomes on January 13th. Both opinions are discussed in greater detail below. OSHA Vaccine-or-Test Mandate In a 6-3...
Read More
How to Detect Employee Burnout and 15 Ways Employers Can Help Reduce It
Employee burnout continues to grow as the global pandemic enters its third year. In fact, experts say burnout is a primary cause for the Great Resignation, in which a record 39 million U.S. workers quit their jobs during the first 10 months of 2021. The root causes of employee burnout...
Read More
DOL Guidance On At-Home COVID-19 Tests
The Departments of Labor, Health and Human Services (HHS), and the Treasury (collectively, the Departments) issued Frequently Asked Questions (FAQs) Monday that generally require group health plans and insurers to cover the costs of at-home over-the-counter COVID-19 tests (OTC COVID-19 Tests) approved by the U.S. Food and Drug Administration (FDA)...
Read More
December 2021 Compliance Recap
December was a quiet month in the compliance world in terms of large announcements, but lots of little information trickled in over the month. OSHA’s vaccine-or-test mandate for large employers and vaccine mandate for health care organizations is headed for the Supreme Court, set to be heard on January 7,...
Read More
Vaccine Mandate for Healthcare Workers Reinstated as U.S. Supreme Court Prepares to Hear Oral Arguments on Vaccine Mandates
The Centers for Medicare and Medicaid Services (CMS) issued an emergency ruling in November 2021, which would require eligible staff at health care facilities participating in Medicare and Medicaid programs to be fully vaccinated against COVID-19. The mandate was quickly challenged in several states, resulting in a nationwide stay on...
Read More
Sixth Circuit Lifts Stay on OSHA COVID-19 Vaccine Mandate for Employers with 100+ Employees
The U.S. Court of Appeals for the Sixth Circuit has issued an opinion lifting the stay on the vaccine-or-test mandate for employers with 100 or more employees. The stay was imposed by the Fifth Circuit Court of Appeals in November as a result of the Emergency Temporary Standard (ETS) released...
Read More
End-of-Year Reminders for Companies with Retirement Plans
As 2021 draws to a close and everyone begins preparing for a new year, employers with qualified retirement plans should review several factors that could affect their plans before moving on to 2022. The fourth quarter presents a perfect opportunity for plan sponsors to take a snapshot of the year’s...
Read More
How to Reset and Reflect After Benefits Renewal Season
The hectic benefits renewal season is finally winding down for many employers, with open enrollment meetings and all the logistical challenges and decisions behind us for 2021. We’re ready to relax, enjoy the holiday season, and move on to new challenges during the new year. But wait a second: maybe we...
Read More
End of Year Employee Benefits Compliance Checklist
From ACA reporting to new federal regulations, employers are faced with several obligations as they close out the year and begin to plan for 2022. To help comply with your obligations, we have complied a list of important items that apply to employer-sponsored group health plans to either review and/or...
Read More
November 2021 Compliance Recap
November saw quite a bit of activity in the compliance space. Although OSHA’s vaccine-or-test mandate for private employers was issued, it was immediately met with resistance in the form of lawsuits and a stay from the Sixth Circuit Court of Appeals. The mandates for federal contractors and health care workers...
Read More
Important Steps to Approach 2022 Strategic Workforce Planning
More employers are turning to workforce planning to provide the necessary information to better manage their talent pool to meet their organization’s strategic needs. The events of the past two years have encouraged more organizations to pay attention to workforce planning as they prepare for the opportunities and possible disruptions...
Read More
Promoting End of Year Workplace Wellness Engagement
As we near the end of the year, don’t let your wellness program slip through the cracks. With the holidays approaching, flu season here, and 2022 planning in full effect, now is the perfect time to evaluate your organization’s end of year wellness initiatives to keep your employees healthy and...
Read More
IRS Proposes Permanent Extension for Distributing ACA Reports
The IRS has issued proposed regulations, which, if finalized, would extend the annual furnishing deadlines for Internal Revenue Code (IRC) Sections 6055 and 6056 reporting under the Affordable Care Act (ACA) permanently. IRC Sections 6055 and 6056 outline reporting requirements for employers and providers to confirm whether individuals have acquired...
Read More
COVID-19 High Deductible Health Plan and IRC Section 125 Changes Expiring in 2022
Provisions in the CARES Act allowed HSA-qualified High Deductible Health Plan (HDHP) participants to receive telemedicine care on a first-dollar basis for plan years beginning on or before December 31, 2021. Additionally, the IRS issued guidance allowing HDHPs to cover the testing and treatment of COVID-19 prior to a participant...
Read More
How We Resolved One Client’s Self-Funding Worries Through Proprietary Confidence Projection
Client Industry: Technology Number of Employees: 240 Service Provided: Statistical risk analysis and probability projections. Challenges Our client had considered transitioning from fully insured to self-funding for several years. Although we projected the change would bring considerable savings, they remained concerned by the risk that the model might not perform...
Read More
Innovative Launches New Resource Page
All good things must come to an end and be replaced with something better! With that being said, Innovative Benefit Planning is thrilled to announce the launch of our new and improved resource page! After months of hard work and devotion to the client experience, we are bringing you a...
Read More
OSHA Suspends Emergency Temporary Standard (ETS) Vaccine Mandate
On November 17, 2021, OSHA suspended the execution and enforcement of its Emergency Temporary Standard (ETS) mandating employers with 100 or more employees to implement mandatory COVID-19 vaccination and testing policies. This suspension came after the Fifth Circuit Court of Appeals granted a motion to stay the mandate until further...
Read More
5 Ways Employers Can Address Mental Health in the Workplace
Mental health is top of mind everywhere these days as about 20% of adult Americans report symptoms of mental illness according to the Centers for Disease Control. Workplace mental health concerns such as anxiety, stress, and depression had already been growing, and then the COVID-19 pandemic and remote work situations...
Read More
IRS Issues 2022 FSA and Commuter Limits
The IRS has announced the 2022 max contribution limits for FSA and Commuter accounts [Revenue Procedure 2021-45]. All FSA and Commuter plans (for the 2022 plan year) will be updated with the 2022 contribution limits. If you have any questions, please contact your account team or email us at icomply@ibpllc.com....
Read More
October 2021 Compliance Recap
October was a relatively quiet month in the compliance space. While we are still waiting for the U.S. government to release the guidance on broker compensation disclosures, here are the highlights of happenings in October. FAQs from the Departments on COVID-19 Vaccines and Employer-Sponsored Group Health Plans On October 4,...
Read More
OSHA Issues Emergency Temporary Standard regarding COVID-19 Vaccine Mandate
On November 5, 2021, the Occupational Health and Safety Administration (OSHA) released the emergency temporary standard (ETS) requiring businesses with at least 100 employees to mandate employee vaccinations or wear masks and be tested for COVID-19 weekly. Employers subject to the vaccine mandate must begin to create a written vaccination...
Read More
Innovative Investment Fiduciaries Receives CEFEX Certification for 3rd Consecutive Year
Over the years, we have worked hard to earn a trusted reputation, which is why we are honored to announce our certification renewal with CEFEX, the Centre for Fiduciary Excellence, LLC, for the third consecutive year. CEFEX is an independent global assessment and certification organization. Its mission is to promote...
Read More
IRS Decreases Federal Affordability Percentage to 9.61% for Plan Years Beginning in 2022
IRS Decreases Federal Affordability Percentage to 9.61% for Plan Years beginning in 2022 Per the Affordable Care Act (ACA), Applicable Large Employers (ALEs), employers with 50 or more full time and/or full-time equivalent employees, are required to offer affordable minimum value coverage to all full-time employees and their dependents. To...
Read More
Innovative Saves Company From a $440,000 Renewal Increase with 45 Days Till Renewal
Challenges A construction company with 100 employees was facing a 29 percent renewal increase for its employee benefits package. The additional cost, which was over $440,000, was much more than the company could absorb. Passing the costs on to the employees through less coverage and higher deductibles seemed like the...
Read More
Departments Issue Further Guidance Under No Surprises Act
On September 30, 2021, the Department of Health and Human Services, the Department of Labor, and the Department of the Treasury (collectively, the Departments), along with the Office of Personnel Management (OPM), released an interim final rule (IFR) under the No Surprises Act (Act) to help protect health care consumers...
Read More
Tamalyn Wandler Joins Innovative as Director of Compliance
Innovative Benefit Planning is pleased to announce that Tamalyn Cee Wandler, JD, has joined our team as Director of Compliance. In her new role, Tamalyn will assist clients with their compliance auditing and educating them on the various federal and state regulations, assess areas of weakness, determine potential liability, and...
Read More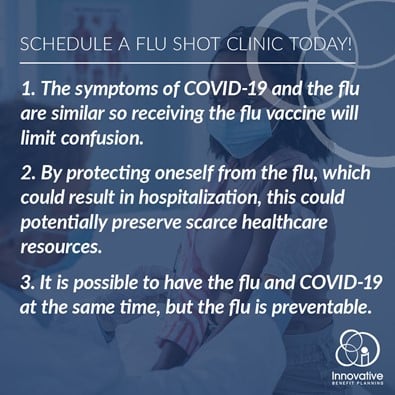
Coordinate Your Flu Shot Clinic Today!
Flu season here and the best way to protect your employees from the flu is to encourage them to get a flu shot! There are always benefits from receiving the flu vaccination, however, due to the ongoing COVID-19 pandemic, this year is more important than ever for your employees to...
Read More
September 2021 Compliance Recap
September saw a lot of activity in the compliance space, especially coming from the federal government. Vaccine Mandate Guidance Still Pending Vaccine mandates were on everyone’s mind, especially after Delta Airlines announced its $200 monthly surcharge and weekly testing program for unvaccinated employees. The government joined the fray when President...
Read More
Employers COVID-19 Vaccine Resources & Kit
Sometimes it’s hard to keep up with all the latest recommendations and regulations. In an effort to ease the burden, we have compiled eight important resources that you can access when planning your COVID-19 vaccine practices. Access Here
Read More
Biden Announces New Vaccination Executive Order
President Joe Biden took aim at vaccine resistance in America, announcing policies requiring most federal employees to get COVID-19 vaccinations and pushing large employers (100+) to have their workers inoculated or tested weekly. The below article outlines more details on these items included in the orders: OSHA is directed to...
Read More
Innovative Launches New Groundbreaking Benefit Performance Assessment
Innovative Launches New Groundbreaking Benefit Performance Assessment Innovative has launched our new groundbreaking, proprietary Benefit Performance Assessment. This complimentary assessment shows employers how they can cut waste, take control of healthcare costs, and provide better service solutions. All within an hour of your time and without impacting the coverage offered...
Read More
Innovative Welcomes Polina Lipskaya as Underwriting Associate
Innovative Welcomes Polina Lipskaya as Underwriting Associate Please join us in welcoming Polina Lipskaya as our newest Underwriting Associate. In this role, Polina will be a key member of the Client Service team. She will directly support the Account Executives, Account Managers, and Consultants with quoting, reporting and the overall...
Read More
ARPA Subsidy Period Expiration Reminder and Updated Guidance
ARPA Subsidy Period Expiration Reminder and Updated Guidance Subsidy Period Expiration Notice ARPA requires subsidy expiration notices to be sent to Assistance Eligible Individuals (“AEIs”) prior to the expiration of the Subsidy Period. This Expiration Notice should be sent no more than 45 days and no less than 15 days...
Read More
Innovative Promotes John Romaska to Vice President of Consulting
Innovative Promotes John Romaska to Vice President of Consulting Innovative Benefit Planning is excited to announce John Romaska has been promoted to Vice President of Consulting. John previously served as our Director of Benefits Consulting, where his responsibilities included strengthening Innovative’s relationships with current clients and overall advancement of the...
Read More
Departments Defer Transparency and Disclosure Rule Enforcement, Provide FAQ Guidance
Departments Defer Transparency and Disclosure Rule Enforcement, Provide FAQ Guidance On August 20, 2021, the U.S. Departments of Health and Human Services, Labor, and Treasury (collectively, the Departments), issued FAQ guidance regarding provisions of the Affordable Care Act (ACA), the No Surprises Act (the Act) and the Consolidated Appropriations Act,...
Read More
No Surprise Billing: Interim Final Regulations Part 2
No Surprise Billing: Interim Final Regulations Part 2 On July 1, 2021, the U.S. Departments of Health and Human Services, Labor, and Treasury, along with the Office of Personnel Management (collectively, the Departments), issued an interim final rule (IFR) to explain provisions of the No Surprises Act (the Act) that...
Read More
Innovative Welcomes Adam Cardell as Executive Account Manager
Innovative Welcomes Adam Cardell as Executive Account Manager We are excited to announce the latest addition to the Innovative Benefit Planning team! Adam Cardell has joined Innovative as an Executive Account Manager. As an Executive Account Manager, Adam will be responsible for strengthening Innovative’s relationships with current clients, as well...
Read More
Innovative Welcomes Carly Vettori to our Team as a Benefits Sales Consultant
Innovative Welcomes Carly Vettori to our Team as a Benefits Sales Consultant We are excited to announce the latest member of Innovative Benefit Planning! Please join us in welcoming Carly Vettori to our team as a Benefits Sales Consultant. In this role, Carly will help us to understand the customer...
Read More
6 Tips for a Healthier Summer BBQ
6 Tips for a Healthier Summer BBQ Grilling is a fun way to prepare some of your favorite foods, especially during the summer. Try out a new recipe and follow these tips to make your summer cooking adventures healthy and flavorful this season! Add color. So many different fruits and...
Read More
Innovative Welcomes Nicoletta Torres as New Account Manager
Innovative Welcomes Nicoletta Torres as New Account Manager We are excited to announce the latest addition to the Innovative Benefit Planning team! Please join us in welcoming Nicoletta Torres as our newest Account Manager. As an account manager, Nicoletta will be a valuable resource to Innovative’s leadership team, employees, and...
Read More
June 2021 Compliance Recap
June 2021 Compliance Recap June 2021 was not a busy month in the benefits industry, largely due to the summer vacation season and the Independence Day holiday. Importantly, however, the U.S. Supreme Court upheld the constitutionality of the Patient Protection and Affordable Care Act (ACA). Additionally, the IRS unveiled a...
Read More
The IRS Issues the Most Recent Update to Form 941
The IRS Issues the Most Recent Update to Form 941 On June 24, 2021, the Internal Revenue Service issued the most recent update to Form 941, the Employer’s Quarterly Federal Tax Return. The form has several new lines added to obtain credits for the COBRA subsidies offered under the American...
Read More
IRS Issues Draft Form 1095-C
IRS Issues Draft Form 1095-C The Internal Revenue Service (IRS) recently issued the 2021 Draft Form 1095-C, which is required to be filed with the IRS by applicable large employers (ALEs), to report the offer of health coverage to employees. New Codes An ALE that offers an individual coverage health...
Read More
EEOC Extends EEO-1 Deadline for 2019 and 2020 Data Submissions
EEOC Extends EEO-1 Deadline for 2019 and 2020 Data Submissions The New Deadline Gives Employers Another Month–Until August 23– To Complete Their Reports Employers now have some extra time to submit equal employment opportunity (EEO-1) workforce data from 2019 and 2020, the U.S. Equal Employment Opportunity Commission (EEOC) announced on...
Read More
Andrew May Promoted to Senior Account Manager – Financial Services
Andrew May Promoted to Senior Account Manager – Financial Services Innovative Benefit Planning is pleased to announce the promotion of Andrew May to Senior Account Manager-Financial Services. Andrew has been a part of the Innovative financial service team for over two years, serving as a Financial Services Associate. During this...
Read More
No Surprise Billing: Interim Final Regulations Part 1
No Surprise Billing: Interim Final Regulations Part 1 On July 1, 2021, the U.S. Departments of Health and Human Services, Labor, and Treasury, along with the Office of Personnel Management (collectively, the Departments), issued an interim final rule (IFR) to explain provisions of the No Surprises Act (the Act) that...
Read More
Benefits of a CEFEX Certified Advisor
Benefits of a CEFEX Certified Advisor A CEFEX (Centre for Fiduciary Excellence) certified advisory firm adheres to a standard representing the best practices in their industry. They abide by a global fiduciary standard of excellence with specific criteria covering 21 best practices. In fact, the documented repeatable processes and the...
Read More
3 Reasons Every Employer Should Benchmark Their Health Plan
3 Reasons Every Employer Should Benchmark Their Health Plan As employers are competing for the race for talent and trying to bend the rising health care cost curve, benchmarking employee benefits is more important than ever. Here are three advantages to benchmarking health benefits: Bragging Rights: Employee benefits are a...
Read More
4 Ways to Leverage National Insurance Awareness Day to Increase Employee Awareness and Participation
June 28th is National Insurance Awareness Day! It was created as a day to review your insurance coverage and is also a great time to help your employees understand the benefits that are available to them. Focus today on empowering your employees to better understand, appreciate and participate in their...
Read More
EEOC Issues Updated COVID-19 Vaccination Assistance
EEOC Issues Updated COVID-19 Vaccination Assistance The Center for Disease Control (CDC) and the Equal Employment Opportunity Commission (EEOC) have issued this information related to vaccinations: Employers must be aware that certain individuals may opt to not be vaccinated, either for religious reasons or for medical reasons Under the Americans...
Read More
Supreme Court Effectively Upholds ACA in Texas v. United States Ruling
Supreme Court Effectively Upholds ACA in Texas v. United States Ruling On June 17, 2021, the U.S. Supreme Court upheld the constitutionality of the Patient Protection and Affordable Care Act (ACA) by a 7-to-2 vote. The Court heard oral arguments in the case, California v. Texas, on November 10, 2020,...
Read More
4 Ways Digital Open Enrollment Guides Improve Employee Engagement
4 Ways Digital Open Enrollment Guides Improve Employee Engagement Every year open enrollment season allows employees to start, stop, or change their existing health insurance plans. Often, however, open enrollment can be a source of confusion, leaving employees with a lack of understanding and underutilizing their plan. Digital open enrollment...
Read More
May 2021 Compliance Recap
May 2021 Compliance Recap May 2021 was a somewhat busy month in the benefits industry. The absence of a significant of amount of agency guidance during the summer months is to be expected. However, the IRS finally issued guidance on the temporary 100% COBRA subsidy mandated by the American Plan...
Read More
Upcoming Challenges with ACA in 2021
Upcoming Challenges with ACA in 2021 IRS Eliminates Transition Relief and Removes Threshold Expanding Eligibility In previous year, the IRS has provided relief of penalties to reporting entities that report incomplete or incorrect information as long as these entities can show they made a good-faith effort to comply with the...
Read More
IRS Draft Form 941 Reflects COBRA Subsidy Tax Credit
IRS Draft Form 941 Reflects COBRA Subsidy Tax Credit The IRS recently released a draft of the revised 2021 version of Form 941, Employer’s Quarterly Federal Tax Return, in order to, in part, reflect the tax credit in connection with the 100% COBRA subsidy under the American Rescue Plan Act...
Read MoreFrequently Asked Questions About the Patient-Centered Outcomes/Comparative Effectiveness (PCORI Fee)
Q1: What plans does the PCORI fee apply to? A1: All plans that provide medical coverage to employees owe this fee. Medical coverage includes preferred provider (PPO) plans, health maintenance organization (HMO) plans, point-of-service (POS) plans, high deductible health plans (HDHPs), and health reimbursement arrangements (HRAs). The fee does not...
Read More
BCBSA Antitrust Settlement Classes Eligible for Proceeds
BCBSA Antitrust Settlement Classes Eligible for Proceeds November 5, 2021 is the deadline for filing a claim in connection with the Blue Cross Blue Shield Association (BCBSA) $2.67 billion settlement reached in October 2020. The class action lawsuit was filed more than eight years ago by subscribers seeking injunctive and...
Read More
2021 Patient-Centered Outcomes Research Institute (PCORI) Fee
2021 Patient-Centered Outcomes Research Institute (PCORI) Fee The Patient-Centered Outcomes Research Institute (PCORI) fee deadline is around the corner. In Notice 2020-84, the IRS adjusted the applicable dollar amount to be multiplied by the average number of covered lives for purposes of calculating the fee for policy years and plan...
Read More
Why Employers Should Benchmark Their Health Plan Before Renewal
Why Employers Should Benchmark Their Health Plan Before Renewal Benchmarking your health plan during renewal ensures that the benefits being offered continue to be a right fit for the company and employees based on data-driven decisions. On the other hand, a poorly planned renewal done in the dark can cause...
Read MoreFrequently Asked Questions About the Patient Centered Outcomes/Comparative Effectiveness (PCORI) Fee
Q1: What plans does the PCORI fee apply to? A1: All plans that provide medical coverage to employees owe this fee. Medical coverage includes preferred provider (PPO) plans, health maintenance organization (HMO) plans, point-of-service (POS) plans, high deductible health plans (HDHPs), and health reimbursement arrangements (HRAs). The fee does not...
Read More
Discover How We Helped One Client Reduce Their Retirement Plan Fees by 30%
Discover How We Helped One Client Reduce Their Retirement Plan Fees by 30% When offering your plan directly with a qualified plan provider, many employers are not aware of what they might be missing. As a result, we often find that many Plan Sponsors are paying more and receiving less....
Read More
IRS Issues 2022 HSA and HRA Limits
IRS Issues 2022 HSA and HRA Limits The IRS issued Revenue Procedure 2021-25 on May 10, 2021, to announce the 2022 inflation adjusted amounts for health savings accounts (HSAs) under Section 223 of the Internal Revenue Code (Code) and the maximum amount that may be made newly available for excepted...
Read More
April 2021 Compliance Recap
April 2021 Compliance Recap April was a busy month in the benefits industry, largely due to the temporary 100% COBRA subsidy mandated by the American Plan Rescue Act of 2021 (the ARP). The Departments of Labor, Treasury and Health and Human Services (the Departments) jointly issued FAQs regarding the amendments...
Read More
5 Steps to Create a Financial Wellness Program
5 Steps to Create a Financial Wellness Program Many employers offer health wellness programs for their organization. However, financial wellness is equally as important. Studies show that 47% of employees are stressed about their finances, which can impact their productivity in the workplace. While starting a financial wellness program may...
Read More
5 Reasons Employers Should Carve Out Prescription Drug Benefits
5 Reasons Employers Should Carve Out Prescription Drug Benefits Prescription Drugs typically makes up 20% of an employer’s overall spend, and with the rise in specialty drugs, industry experts expect that number to encroach 50%. Employers have the ability to “carve-out” this coverage from their medical plan, resulting in significant...
Read More
Innovative Launches New Online Health Plan Benchmarking Tool
Innovative Launches New Online Health Plan Benchmarking Tool Benchmarking is more important than ever. Knowing how your health plan compare to your peers allows you to be competitive in recruiting and retaining the best employees, assist with making data-driven decisions during renewal planning, and see how your health plan costs...
Read More
Innovative Launches New Digital Employee Benefit Guide Technology
Innovative Launches New Digital Employee Benefit Guide Technology As technology continues to transform the workplace, HR professionals are seeking new and improved ways to deliver their health plan benefits, while gaining rich backend intelligence to improve the utilization of the plan. We have the solution! Innovative Benefit Planning is excited...
Read More
The DOL Issues ARPA COBRA Subsidy Forms
The DOL Issues ARPA COBRA Subsidy Forms On April 7, 2021, the Department of Labor (DOL) issued the much awaited COBRA Model Notices required under the American Rescue Plan Act of 2021 (ARPA), implementing the 100% COBRA Subsidy for eligible individuals. In order to assist plan sponsors with implementing the...
Read More
Environmental, Social and Governmental (ESG) Fund Best Practices for Plan Sponsors
Environmental, Social and Governmental (ESG) Fund Best Practices for Plan Sponsors Socially responsible investing has grown in popularity as investors become more aware of how organizations operate from an environmental, social and governance perspective. Environmental factors may include a company’s carbon output, overall resource consumption and impact to air and...
Read More
March 2021 Compliance Recap
March 2021 Compliance Recap The employee benefits guidance issued in March 2021 was largely focused on providing relief to individuals and businesses impacted by the continuing COVID-19 pandemic. Significantly, on March 11, 2021, the American Rescue Plan Act of 2021 (the Act) was enacted into law which, in part, mandates...
Read More
Innovative’s 2020 Consulting Highlights
Innovative’s 2020 Consulting Highlights 2020 was a challenging year for many, but here at Innovative, we were dedicated to delivering the best value and results for our clients. Not only were we successful in reducing costs for our clients, but we were able to provide them with a number of...
Read More
PPE as Section 213(d) Qualified Medical Expenses
PPE as Section 213(d) Qualified Medical Expenses The Internal Revenue Service (IRS) released Announcement 2021-7 providing that amounts paid for personal protective equipment (PPE) such as masks, hand sanitizer and sanitizing wipes, for the primary purpose of preventing the spread of COVID-19, are qualified medical expenses under Internal Revenue Code...
Read More
American Rescue Plan Act Brings Several Health Plan Provisions
On March 11, 2021, President Biden signed the American Rescue Plan Act of 2021 (Act). The Act is a $1.9 trillion legislative package that includes pandemic relief for individuals and families. The Act contains several provisions including funding to the Centers for Disease Control and Prevention, stimulus checks, unemployment benefits,...
Read More
Is Level Funding a Good Fit for Your Employee Benefits Plan?
Is Level Funding a Good Fit for Your Employee Benefits Plan? Level funding is a great strategy for employers that are interested in self-funding, but like a plan that looks and feels like it is fully insured. Level funding acts just like a fully insured plan, except it provides the...
Read More
February 2021 Compliance Recap
February 2021 Compliance Recap February was a relatively busy month in the employee benefits world. The Department of Labor (DOL) issued EBSA Disaster Relief Notice 2021-01 regarding the end of the COVID-19 outbreak period. The Internal Revenue Service (IRS) issued Notice 2021-15 providing guidance on health flexible spending arrangements (FSAs),...
Read More
Final Rule on the Extension of Certain Timeframes For Employee Benefit Plans, Participants, and Beneficiaries Due to COVID-19
Final Rule on the Extension of Certain Timeframes For Employee Benefit Plans, Participants, and Beneficiaries Due to COVID-19 The DOL issued EBSA Disaster Relief Notice 2021-01 providing that the outbreak period relief noted below ends on the earlier of one year from the date an individual or plan was first...
Read More
Incorporating Wellness into Your Employee Benefits Strategy
Incorporating Wellness into Your Employee Benefits Strategy Wellness is a strategy that continues to gain in popularity as employers are looking for ways to help their employees become healthier, more engaged, and happier at work. Wellness is typically broken into three categories. The first category is educational wellness. With an...
Read More
Reference Based Pricing
Reference Based Pricing With healthcare costs skyrocketing at unsustainable levels, employers are considering nontraditional methods of funding their medical plans. One nontraditional method that employers are starting to consider is called reference based pricing, or RBR. This method has proven to reduce overall benefit spend 20 to 30%, when compared...
Read More
Innovative Launches Employee Management Training; PeopleForce 2030
Innovative Launches Employee Management Training; PeopleForce 2030 Innovative Benefit Planning, LLC is excited to launch PeopleForce 2030, a three-part employee training series consisting of facilitated and interactive 90-minute sessions that discuss leadership competencies including “Interpersonal Savvy”, “Dealing with Ambiguity”, and “Building Resilience”. Whether your employees are charged with leading and...
Read MoreInnovative Launches COVID-19 Employee Monitoring and Advocacy Solution
Innovative Launches COVID-19 Employee Monitoring and Advocacy Solution Innovative Benefit Planning, LLC is here to help your organization bring your employees back to the workplace safely and securely. In order to so, we are proud to launch our COVID-19 Employee Health Tracker, which will provide employers a COVID-19 monitoring and...
Read More
What is Bundled Pricing?
What is Bundled Pricing? Many employers are frustrated with a lack of financial and quality transparency in the healthcare marketplace. As such, many employers have considered offering a bundled pricing solution to their employees. Bundled pricing is a unique solution that provides employees the opportunity to shop for a procedure...
Read More
January 2021 Compliance Recap
January 2021 Compliance Recap January was a busy month in the employee benefits world. President Biden issued a memorandum putting a regulatory freeze on new rules. President Biden also issued an executive order on strengthening Medicaid and the Patient Protection and Affordable Care Act (ACA). The Department of Labor (DOL)...
Read More
Understanding Captives and Consortiums
Understanding Captives and Consortiums As health insurance costs continue to rise, many small and mid-size employers have looked for ways to alternatively fund their plans and potentially save costs. Self-funding can be daunting and unmanageable for many small to mid-size employers, but there are many self-funding options to consider. Captives...
Read More
EEOC Releases Proposed Wellness Rules under ADA and GINA
EEOC Releases Proposed Wellness Rules Under ADA and GINA The EEOC recently released proposed language revising the wellness incentive rules under the ADA and GINA. This proposed language is a revision to the rules released in 2016. Below is a summary of the proposed changes and how they may impact...
Read More
2021 Minimum Wage Increases
2021 Minimum Wage Increases As of January 1, 2021, several US states increased their minimum wage rate. Please note, however, that some cities or municipalities may have a minimum wage rate even greater than their statewide rate. Below outlines effective wages for states where the rate will be changing. Alaska:...
Read More
December Compliance Recap
December was a busy month in the employee benefits world. President Trump signed the Consolidated Appropriations Act, 2021, which includes the No Surprises Act and other group health plan provisions. The Centers for Disease Control Advisory Committee on Immunization Practices (ACIP) issued two interim recommendations for COVID-19 vaccines. The Department...
Read More
2021 Plan Sponsor Considerations
The events of 2020 created many new considerations for plan sponsors as individuals were faced with uncertainty and sought safety both financially and personally. The CARES Act was passed to assist individuals and businesses impacted by the pandemic, and investors witnessed a volatile investment market causing many to adjust their...
Read More
Consolidated Appropriations Act, 2021: Temporary Health FSA and DCAP Relief
Consolidated Appropriations Act, 2021 Temporary Health FSA and DCAP Relief The Consolidated Appropriations Act, 2021 (Appropriations Act), enacted on December 27, 2020, contains temporary rules to provide relief for participants in health flexible spending arrangements (FSAs) and dependent care flexible spending arrangements (DCAPs) in light of the COVID-19 pandemic. The...
Read More
Mandatory Coverage of COVID-19 Vaccines under Group Health Plans
Mandatory Coverage of COVID-19 Vaccines Under Group Health Plans On December 11, 2020, the Food and Drug Administration (FDA) issued an Emergency Use Authorization for the Pfizer-BioNTech COVID-19 vaccine (Pfizer vaccine). The following day, December 12, 2020, the Centers for Disease Control Advisory Committee on Immunization Practices (ACIP) issued an...
Read More
Congress Passes New $1.4 Trillion Stimulus & COVID-19 Relief Bill and Awaits President’s Signature
Congress Passes New $1.4 Trillion Stimulus & COVID-19 Relief Bill and Awaits President’s Signature Details have emerged on the new $1.4 trillion omnibus spending bill which provides a $900 billion COVID-19 Stimulus package. The bill awaits President Trump’s signature and as of last night, he requested that Congress amend the...
Read More
Blue Cross Blue Shield Association Tentative $2.67 Billion Antitrust Settlement
Blue Cross Blue Shield Association Tentative $2.67 Billion Antitrust Settlement Blue Cross Blue Shield Association (BCBSA) has recently reached a tentative $2.67 billion settlement arising out of a class action lawsuit filed more than eight years ago by subscribers seeking injunctive and compensatory relief arising out of BCBSA’s alleged violation...
Read More
Healthy for the Holidays
Healthy for the Holidays Tis’ the Season for Temptations While the holidays are an exciting and eventful time of year, holiday festivities can often revolve around eating and drinking. Traditions involve baking cookies, high calorie drink making, and eating plentiful holiday meals. We tend to get so busy around this...
Read More
November Compliance Recap
November Compliance Recap November was a relatively busy month in the employee benefits world. The U.S. Supreme Court (Supreme Court) heard oral arguments in the case of California v. Texas, which is the case challenging the constitutionality of the ACA. The Internal Revenue Service (IRS) released the updated Patient-Centered Outcomes...
Read More
Partially Self-Funded Plans with an HRA
Partially Self-Funded Plans with an HRA As health insurance costs continue to rise, more and more small and mid-size employers are looking for ways to take control of their healthcare costs. A health reimbursement account, or an HRA, is a way in which employers can step into self-funding and start...
Read More
Fostering Company Culture in a Remote Environment
Fostering Company Culture in a Remote Environment It has been a challenging year for all of us, to say the least. Many businesses were forced to make the move to a remote environment, while others have maintained in-person operations with serious restrictions on gatherings. While business as we know it...
Read More
Updated PCORI Fee Released
Updated PCORI Fee Released Employers that sponsor certain self-insured health plans are responsible for Patient-Centered Outcomes Research Institute (PCORI) fees. Under the Affordable Care Act, PCORI fees were originally scheduled to apply to policy or plan years ending on or after Oct. 1, 2012 and before Oct. 1, 2019. However, in Dec....
Read More
How to Host a Virtual Company Holiday Party
How to Host a Virtual Company Holiday Party This holiday season may be different for many organizations than it has in the past, but that doesn’t mean that the holidays need to be disregarded all together. One thing is for certain, and that is that your team has worked diligently...
Read More
Free Child Education Resources
Free Child Education Resources As most children are learning virtually as a result of the COVID-19 pandemic, many parents are looking to compliment their education with additional resources. Especially now, there are a great deal of free resources available for all subject matter. Check out some of the most popular...
Read More
End of Year Wellness Initiatives to Drive Employee Well-Being
End of Year Wellness Initiatives to Drive Employee Well-Being As we near the end of the year, don’t let your wellness program slip through the cracks. With the holidays approaching, flu and germ season here, and 2021 planning in full effect, now is the perfect time to evaluate your organization’s...
Read More
Understanding Key Health Insurance Terms
Understanding Key Health Insurance Terms The language of health insurance can be confusing but understanding some key terms will help your employees comprehend the basics of your organization’s plan, allowing them to make smart decisions that will benefit their family. Rather than feeling confused, encourage them to review the following...
Read More
The CDC Redefines “Close Contact”
The CDC Redefines “Close Contact” As the number of reported cases of COVID-19 continues to rise, employers are increasingly confronted with questions and obligations regarding their workforce. With that being said, employers should be aware that as of October 21st, the CDC revised the definition of “close contact” to include...
Read More
October Compliance Recap
October was a busy month in the employee benefits world. The Department of Health and Human Services (HHS) renewed the public health emergency due to COVID-19 which took effect on October 23, 2020. The Internal Revenue Service (IRS) issued Notice 2020-76 regarding deadline extensions and requirements for reporting of group...
Read More
Final Rules on Coverage Transparency
Final Rules on Coverage Transparency On October 29, 2020, the Internal Revenue Service (IRS), Department of Labor (DOL), and the Department of Health and Human Services (HHS) (collectively, Departments), released final rules on coverage transparency, in order to provide health coverage recipients with an estimate of their potential cost-sharing liability...
Read More
Better Sleep for Better Health
Better Sleep for Better Health As we approach the holiday season, it is important to remember to take some time to care for yourself. The holidays can be extremely busy, stressful, and even draining at times. Don’t forget to make yourself a priority. Self-care is about taking time for yourself,...
Read More
6 Self-Funding Strategies to Suit Your Needs
6 Self-Funding Strategies Self-funding is nothing new as it has been a common form of health plan financing since 1974. Self-funding provides great flexibility with plan designs and provides freedom from most state laws. In fact, over 60% of US employees are covered under a self-insured medical plan. Under self-funded...
Read More
NJ Employers Must Adhere to Latest Executive Orders Mandating Health and Safety Protocols for COVID-19
NJ Employers Must Adhere to Latest Executive Orders Mandating Health and Safety Protocols for COVID-19 On October 28, 2020, New Jersey Governor Phil Murphy signed Executive Order No. 192 (EO 192), which mandates that New Jersey employers abide by certain health and safety standards in an effort to protect employees...
Read More
IRS Announces 2021 Plan Limitations
IRS Announces 2021 Plan Limitations The IRS has recently announced the qualified plan limitations for 2021, which are determined based on annual increases in the cost of living index. Because there was only a modest increase in the index, most of the plan limits have not changed from 2020. For...
Read More
How Working With a Qualified Plan Advisor Can Improve Your Audit Experience
How Working With a Qualified Plan Advisor Can Improve Your Audit Experience Hiring a quality qualified plan advisor provides many advantages to employers that sponsor a retirement plan. Specifically, one of those advantages is improving your annual qualified plan audit. As each audit season begins, employers often dread having to...
Read More
2021 IRS Contribution Limits for FSA and Commuter Benefits
2021 IRS Contribution Limits for FSA and Commuter Benefits On Tuesday, the IRS released 2021 contribution limits for medical FSA and Commuter Benefits for 2021. There are no changes to flexible spending account (FSA) and commuter benefits contribution limits for 2021. The IRS did adjust the contribution limits for adoption...
Read More
CARES ACT & FFCRA Tax Credits for Eligible Employers
CARES ACT & FFCRA Tax Credits for Eligible Employers Eligible employers are entitled to receive a credit in the full amount of the required sick leave and family leave, plus related health plan expenses and the employer’s share of Medicare tax on the leave, for the period of April 1,...
Read More
3 ACA Reporting Errors and The Pandemic’s Impact
3 ACA Reporting Errors and The Pandemic’s Impact As we approach the end of 2020, we must consider how the various enrollment fluctuations due to the COVID-19 Pandemic will impact the ACA Employer Mandate and the already tedious 1095/1094 ACA Reporting. The IRS recently granted a March 2nd deadline extension...
Read More
September Compliance Recap
September Compliance Recap September was a relatively quiet month in the employee benefits world. President Trump issued an executive order on An America-First Healthcare Plan, noting the Administration’s actions on healthcare and planned actions going forward. A federal district court halted the repeal of certain provisions of the prior final...
Read More
Have You Received an MLR Rebate Check? What To Do Next?
Have You Received an MLR Rebate Check? What To Do Next? The Affordable Care Act requires health insurance carriers to spend at least 80-85 percent of premium dollars on medical care and healthcare quality improvement. If the carrier does not meet this medical loss ratio (MLR) obligation, it must give...
Read More
Dust Off That Old Policy: Why Now is a Good Time to Review Your Life Insurance Policies
Dust Off That Old Policy: Why Now is a Good Time to Review Your Life Insurance Policies As a result of the COVID-19 National Emergency, insurance companies have modified their underwriting requirements to help individuals secure additional life insurance protection. Through new “relaxed” underwriting guidelines, insurers are offering coverage without...
Read More
IRS Extends ACA Reporting Deadline for Furnishing Statements for 2020 from February 1 to March 2, 2021
IRS Extends ACA Reporting Deadline for Furnishing Statements for 2020 from February 1 to March 2, 2021 As the deadline for reporting of group health coverage offered in 2020 under the Patient Protection and Affordable Care Act (ACA) approaches, the Internal Revenue Services (IRS) has issued IRS Notice 2020-76 (Notice)...
Read More
How Employers Can Show Support on World Mental Health Awareness Day
How Employers Can Show Support on World Mental Health Awareness Day World Mental Health Day is recognized annually to promote education for global mental health, as well as create awareness and advocacy against social stigma. This yearly observance has occurred since 1992 and carries with it a yearly theme. It...
Read More
Participant Risk Assessment
Participant Risk Assessment As we work our way through a market recovery and closer to what could be a greater period of uncertainty around the upcoming election, now may be a good time for participants to review the equity risk associated with their retirement account and understand if their current...
Read More
New FAQs Address Questions Employers May Ask to Screen Employees for COVID-19 and ADA Requirements for Handling Employees’ Medical Information
New FAQs Address Questions Employers May Ask to Screen Employees for COVID-19 and ADA Requirements for Handling Employees’ Medical Information On Sept. 8, 2020, U.S. Equal Employment Opportunity Commission (EEOC) issued additional answers to frequently asked questions (FAQs) about how employers should comply with the Americans with Disabilities Act (ADA)...
Read More
August Compliance Recap
August 2020 Compliance Recap August was a relatively busy month in the employee benefits world. The Congressional Research Service (CRS) released an updated report on health savings accounts (HSAs) that summarizes the principal rules governing HSAs and changes made to HSAs as a result of the COVID-19 pandemic. The Department...
Read More
What Steps Can Plan Sponsors and Retirement Plan Committee Members Take to Protect Themselves?
What Steps Can Plan Sponsors and Retirement Plan Committee Members Take to Protect Themselves? When managing a qualified retirement plan, there are certain duties the plan sponsor and committee members have to the plan and participants as named fiduciaries. These duties create liability for the plan sponsor and committee members...
Read More
July Compliance Recap
July was a busy month in the employee benefits world. The U.S. Supreme Court (Supreme Court) upheld the religious exemption and moral exemption final rules to the Patient Protection and Affordable Care Act (ACA) contraceptive mandate. The Internal Revenue Service (IRS) released the indexed 2021 ACA affordability percentage. The President...
Read More
Return to Work Training Kit
Return to Work Training Kit Bring your employees back to work safely with our “Return to Work Training Kit.” Innovative has developed two training tools that you can use in conjunction with each other to educate your employees on what you are doing in response to COVID-19, understand what they...
Read More
Important Plan Considerations Regarding FSA Mid-Year Changes
Important Plan Considerations Regarding FSA Mid-Year Changes As you are aware, in order to provide additional relief to Americans during these challenging times, the IRS released Notice 2020-29 and 2020-33. These notices provided new relaxed rules for 2020 that affected Health Flexible Spending Accounts (FSAs). As a reminder if you...
Read More
Put Your Advisor to the Test
Put Your Advisor to the Test Ask these critical questions to test the knowledge of future plan advisors. A knowledgeable plan advisor is an important component in the successful operation of your qualified plan. However, selecting the right candidate requires more than simply reviewing typical Request for Proposal (RFP) responses....
Read More
Becoming Sun Sensible This Summer
Becoming Sun Sensible This Summer According to skincancerprevention.org, every year in the U.S. nearly 5 million people are treated for skin cancer. Exposure to ultraviolet (UV) light is a major risk factor for most skin cancers, so sun safety is extremely important. Skin cancers start when UV rays damage the...
Read More
June Compliance Recap
June was a busy month in the employee benefits world. The Internal Revenue Service (IRS) released the updated patient-centered outcomes research institute (PCORI) fee amount and announced transition relief. The Department of Health and Human Services’ Office for Civil Rights (OCR) published a final rule regarding the Patient Protection and...
Read More
PCORI Fees are Extended an Additional 10 Years
PCORI Fees are Extended an Additional 10 Years As a reminder, employers that sponsor certain self-insured health plans are responsible for Patient-Centered Outcomes Research Institute (PCORI) fees. Fees for plan years that ended in 2019 are due July 31, 2020. Under the Affordable Care Act, PCORI fees were originally scheduled to apply...
Read More
Judge Rules for HHS in Price Transparency Case
Judge Rules for HHS in Price Transparency Case A federal judge ruled against the American Hospital Association (AHA) on Tuesday in its lawsuit attempting to block an HHS rule pushing for price transparency. The judge ruled in favor of the department, which requires hospitals to reveal private, negotiated rates with insurers beginning...
Read More
DOL Launches Online Tool to Help Employees Determine FFCRA Eligibility
DOL Launches Online Tool to Help Employees Determine FFCRA Eligibility The U.S. Department of Labor launched an interactive online tool to help workers determine if they qualify for paid sick leave or extended family and medical leave to cover time away from work for reasons related to the coronavirus. The tool guides...
Read More
President Trump Signs Paycheck Protection Flexibility Act
President Trump Signs Paycheck Protection Flexibility Act The President authorized the Paycheck Protection Flexibility Act on June 5th after it was passed by the House on May 28th with only one dissenting vote and passed unanimously by the Senate on June 3rd. This act changes provisions surrounding loan forgiveness through...
Read More
May Compliance Recap
May was a busy month in the employee benefits world. The Internal Revenue Service (IRS) issued IRS Notice 2020-29 that provides increased flexibility for making mid-year elections or changes under a Section 125 cafeteria plan during calendar year 2020 and provides increased flexibility to apply unused amounts in health flexible...
Read More
HSA Limits Released for 2021
IRS issued the 2021 cost-of-living adjustments for Health Savings Accounts and High Deductible Health Plans. 2020 2021 Self-Only Contribution Limit $3,550 $3,600 Family Contribution Limit $7,100 $7,200 HDHP – self-only coverage Annual deductible not less than: Annual out-of-pocket expenses do not exceed: $1,400 $1,400...
Read More
COVID-19 Impact on Retirement Plan Discrimination Testing
COVID-19 Impact on Retirement Plan Discrimination Testing As a result of COVID-19, many employers have made financial, operational, and employment-related changes. Plan sponsors need to consider how the following actions may impact the results of their 2020 retirement plan discrimination testing: Changing or Discontinuing the employer 401K match Retirement plan...
Read More
Paycheck Protection Program (PPP) Loan Forgiveness Application
Paycheck Protection Program (PPP) Loan Forgiveness Application On Friday, May 15th the SBA has released their forgiveness application with detailed instructions on how to complete the form. While the release promised further guidance on loan forgiveness, Innovative has received a lot of questions surrounding the calculation of Full Time Equivalent (FTE)...
Read More
Further Guidance on Internal Revenue Service Notice 2020-29
Further Guidance on Internal Revenue Service Notice 2020-29 The Internal Revenue Service (IRS) issued IRS Notice 2020-29 (Notice) that provides increased flexibility for making mid-year elections or changes under a Section 125 cafeteria plan during calendar year 2020 related to employer-sponsored health coverage, health flexible spending arrangements (health FSAs), and...
Read More
April Compliance Recap
April was a busy month in the employee benefits world. The President signed the Paycheck Protection Program and Health Care Enhancement Act (PPPHCEA). The Department of Labor (DOL) and the Department of the Treasury (Treasury) released a final rule extending certain timeframes under the Employee Retirement Income Security Act (ERISA)...
Read More
IRS Releases Two New COVID-19 Notices
IRS Releases Two New COVID-19 Notices To provide additional relief to Americans during these challenging times, the IRS released Notice 2020-29 and 2020-33. These notices provided new relaxed rules for 2020 for making elections under Cafeteria plans, using amounts during a grace period or carryover period changes to the method...
Read More
Open Enrollment and Outcomes Based Health Screenings Options During COVID-19
Open Enrollment and Outcomes Based Health Screenings Options During COVID-19 Due to the COVID-19 outbreak, employers who were planning on offering on-site health screenings tied to payroll deductions are unfortunately being forced to consider other options. Thankfully, the screening vendors have been flexible with delaying screening dates. As an employer,...
Read More
Final Rule on the Extension of Certain Timeframes for Employee Benefit Plans Due to COVID-19
On March 13, 2020, President Trump issued the Proclamation on Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak and by separate letter made a determination, under Section 501(b) of the Robert T. Stafford Disaster Relief and Emergency Assistance Act, that a national emergency exists nationwide beginning March...
Read More
Paycheck Protection Program and Health Care Enhancement Act
Paycheck Protection Program and Health Care Enhancement Act In response to the spread of the 2019 novel coronavirus (COVID-19), President Trump signed the Paycheck Protection Program and Health Care Enhancement Act (PPPHCEA) into law on April 24, 2020. The PPPHCEA is phase 3.5 in Congress’ response to the COVID-19 pandemic...
Read More
4 Tips for a Volatile Market
The COVID-19 National Emergency has impacted nearly every part of our daily lives and the investment market is no exception. When account balances fluctuate, it is tempting to make quick investment decisions. Before you do, consider a few investing tips to guide your investments through volatile markets. Remain Calm Many...
Read More
Relaxed Life, Disability and Long-Term Care Insurance Underwriting
As a result of the COVID-19 National Emergency, insurance companies have adapted to help individuals easily secure protection and obtain insurance without a medical exam that requires a nurse to visit your home or office. This is a TEMPORARY change that will likely end when social distancing can stop. How...
Read More
Innovative Welcomes Lauren Urbanski as Executive Account Manager
Innovative Welcomes Lauren Urbanski as Executive Account Manager We are excited to announce our newest member of the Innovative team, Lauren Urbanski! Lauren joins Innovative as an employee benefits Executive Account Manager. In this role, Lauren is responsible for strengthening and maintaining Innovative Benefit Planning’s relationships with its current clients...
Read More
March Compliance Recap
March was a busy month in the employee benefits world. The President signed the Families First Coronavirus Response Act (FFCRA) into law. The Department of Labor (DOL) issued a bulletin regarding enforcement of the FFCRA. The President also signed the Coronavirus Aid, Relief, and Economic Security Act (CARES Act) into...
Read More
Gov. Murphy Signs Executive Order Granting Grace Periods for Insurance Premium Payments
Gov. Murphy Signs Executive Order Granting Grace Periods for Insurance Premium Payments On April 9, 2020, New Jersey Governor Phil Murphy signed Executive Order No. 123, extending grace periods during which certain insurance companies, including health and dental insurers, life insurers, and property and casualty insurers, will not be able to...
Read More
Stress Management Tips
Stress Management Tips Maintaining your mental and emotional health is essential, and it’s more important than ever to take care of yourself and embrace activities that will help bring you a sense of calm and well-being. Here are some practical tips which will help: Sleep. Make sure you are getting...
Read More
COVID-19 Employer Considerations Regarding Employment Decisions and Plan Coverage Changes
Due to the recent national health crisis in our country, many employers are considering the best way to handle a temporary economic turndown to best position themselves for recovery once the pandemic ceases and businesses can begin to return to some sense of normalcy. In addition, many employers are also...
Read More
CARES Act: Loans & Tax Credit Provisions
CARES Act: Loans & Tax Credit Provisions On March 27, 2020, Congress passed, and the President signed, an unprecedented 2 trillion-dollar stimulus and relief package into law, named the Coronavirus Aid, Relief, and Economic Security Act or the CARES Act. This act provides direct stimulus relief to corporations and individuals....
Read More
CARES Act: Impact on your Retirement Plans
CARES Act: Impact on your Retirement Plans The CARES Act is the stimulus package the government recently enacted to support the country and economy during and after the coronavirus pandemic. The 880-page Act has many programs and features that affect a wide range of the economy. The points below are...
Read More
CARES Act: Impact on Employee Benefits
CARES Act: Impact on Employee Benefits On March 27, 2020, Congress passed, and the President signed, an unprecedented 2 trillion-dollar stimulus and relief package into law, named the Coronavirus Aid, Relief, and Economic Security Act or the CARES Act. This act provides direct stimulus relief to corporations and individuals. While...
Read More
Telemedicine Wait Times
In light of the recent COVID-19 (coronavirus) outbreak. The CDC recommends leveraging telemedicine for your unique medical needs to help limit the spread of the virus by eliminating the risk of exposure to the ER, urgent care, and primary care offices. They are recommending members schedule their virtual visits rather...
Read More
Student Loan Relief Due to COVID-19
Overview On March 13, 2020, the U.S. Department of Education announced that it would waive interest charges, allow for suspended payments and provide assistance to borrowers of defaulted loans for 6 months. All information can be found at StudentAid.gov. Who Is Affected? All borrowers who have an outstanding federal student...
Read More
Market Performance: Tips for Addressing Employee Concerns and Prudent Plan Management
The coronavirus (COVID-19) pandemic and recent market volatility have undoubtedly presented you with new challenges as you care for your employees, families and community. We encourage you to lean on Innovative Investment Fiduciaries as a source for stability during these times. Below is our recent plan sponsor brief with some...
Read More
CARES Act Provisions
On March 27, 2020, Congress passed, and the President signed, an unprecedented 2 trillion dollar stimulus and relief package into law. The law’s nearly 900 pages provide relief for specific industries, including hospitals, airlines, and railroads, as well as cash payments to individuals of up to $1,200 per adult and...
Read More
DOL Issues Families First Coronavirus Response Act Model Notice
DOL Issues Families First Coronavirus Response Act Model Notice As required by the Families First Coronavirus Response Act, the Department of Labor has issued a model notice to be posted by employers. The notice is attached here, and should be posted or distributed to employees in its entirety. To assist...
Read More
Families First Coronavirus Response Act
On March 18, 2020, the President signed into law the Families First Coronavirus Response Act. While largely the same as the House bill passed on March 13, the final version of the legislation differs in several material respects from the original legislation, including permitting exemptions for employers with fewer than...
Read More
COVID-19: Leave Donation Program
Leave donation programs have been considered and implemented by employers for years to allow employees to donate accrued paid time (PTO), vacation or sick leave to a general pool. The time available in this pool serves to be used by fellow employees who have medical emergencies or who are affected...
Read More
COVID-19: Carrier Enhancements
COVID-19: Carrier Enhancements March 17th, 2020 Due to the outbreak of COVID-19 in the United States, the CEO’s of major US health insurance companies met at the White House on March 10, 2020 and agreed to waive costs for certain services such as the COVID-19 test, telemedicine services and prescription...
Read More
Families First Coronavirus Response Act
Families First Coronavirus Response Act On March 18, 2020, the President signed into law the Families First Coronavirus Response Act. While largely the same as the House bill passed on March 13, the final version of the legislation differs in several material respects from the original legislation, including permitting exemptions...
Read More
COVID-19: Tips and Prevention
COVID-19: Tips and Prevention Employees may have questions about what they can do to help manage the situation, and as an employer, you want to be proactive in communicating how to prevent the spread of the virus in the workplace. Innovative has created an easy to download infographic that can...
Read More
COVID-19: 7 Important Employer Considerations
COVID-19: 7 Important Employer Considerations As employers prepare for COVID-19 accommodations, Innovative has developed a checklist that offers specific considerations for employers in planning for emergencies like COVD-19. Examples include policies to review, communication strategies to consider and benefits that may be impacted. The Innovative team is here to support...
Read More
ACA Filings for Employers with NJ Resident Employees Due 3/31
ACA Filings for Employers with NJ Resident Employees Due 3/31 March 16th, 2020 As you may be aware, as of January 1, 2019 the State of New Jersey enacted a mandate requiring New Jersey residents to maintain Minimum Essential Health Coverage, mirroring the requirements of the federal Affordable Care Act. As...
Read More
COVID-19 Communicating With Employees
COVID-19 Communicating with Employees March 12th, 2020 As part of their efforts to prevent the spread of COVID-19 in the workplace, employers should implement an employee communication plan about the illness to employees. The CDC, WHO and OSHA have all created informational material on the virus and its symptoms, prevention...
Read More
Coronavirus And The Workplace
Coronavirus And The Workplace March 12th, 2020 Dealing with Epidemics and Communicable or Infectious Diseases As the number of reported cases of the novel Coronavirus (COVID-19) continues to rise, employers are increasingly confronted with the possibility of an outbreak in the workplace. Employers are obligated to maintain a safe and...
Read More
February 2020 Compliance Recap
February was a busy month in the employee benefits world. The Centers for Medicare and Medicaid Services (CMS) released an updated Premium Assistance Under Medicaid and the Children’s Health Insurance Program (CHIP) model notice. CMS also issued frequently asked questions (FAQs) regarding its recently issued summary of benefits and coverage...
Read More
Terriann Procida Invited to Join Philadelphia Business Journal Leadership Trust
Terriann Procida, CEO, has been invited to join Philadelphia Business Journal Leadership Trust, an exclusive community for influential business leaders, executives and entrepreneurs in Greater Philadelphia. Terriann was chosen for membership by the Philadelphia Business Journal Leadership Trust Selection Committee due to her experience, leadership and influence in the local...
Read More
Proposed Mandatory Anti-Harassment Policy Development and Training Delivery in the State of New Jersey
Proposed Mandatory Anti-Harassment Policy Development and Training Delivery in the State of New Jersey March 4th 2020 On February 18, 2020 New Jersey Governor Phil Murphy presented a new bill to the State Legislature that would require all public and private employers in the state to develop anti-harassment policies and...
Read More
Eat Right, Bite By Bite
Eat Right, Bite By Bite March 3rd, 2020 The key to achieving optimal health cannot be found in any one food, drink or pill, but rather through your personal commitment to healthy lifestyle behaviors. Focusing on maintaining and enjoying good nutrition and daily physical activity is the key to success....
Read More
Ways Employers Can Deal With Employee Student Loan Debt
Ways Employers Can Deal With Employee Student Loan Debt February 25th, 2020 Student debt has increased dramatically in recent years, creating a financial burden on employees’ ability to save for retirement. Many employers have begun implementing programs to help employees manage student loan debt. Millennials (and their families) are often...
Read More
4 Concepts to Construct Company Culture
4 Concepts to Construct Company Culture February 25th, 2020 When we think of employee retention, it often seems like we think of the same few strategies: employee benefits, PTO, food, etc. However, the company culture surrounding a team seems to matter just as much. Your employees spend a considerable amount...
Read More
January 2020 Compliance Recap
January was a busy month in the employee benefits world. The U.S. Supreme Court (Supreme Court) denied expedited review of a court case challenging the constitutionality of the Patient Protection and Affordable Care Act (ACA). The Supreme Court also granted review of a nationwide preliminary injunction of the November 2018...
Read More
Heart Health Month: Show Yourself Some Love
February is heart health month and it’s a great time to raise awareness and learn what you can do to reduce your risk of heart disease. Because many cases of heart disease are controllable, you can take charge of your health by actively working to improve it by making some...
Read More
DOL Increases ERISA Penalties for 2020
January 29th, 2020 On January 15, 2020, consistent with its policy of annual adjustment, the DOL published its final rule adjusting ERISA’s civil monetary penalties for 2020. ERISA protects the interests of employee benefit plan participants and their beneficiaries. The adjustments are non-discretionary (and therefore not subject to a notice...
Read More
How Managers Can Influence Workplace Well-Being
How Managers Can Influence Workplace Well-Being January 16th, 2020 When you think about your best manager, what are the first few things that come to mind? Hopefully, you think about someone who is bold, communicates well, gives employees space to do great work and positions them to take care of themselves. When it comes to well-being, managers...
Read More
New Year, New You
Bring on the best you, this year! Wondering how you can stick to your goals this year? The key to making a healthy change is to set yourself up for success. Your changes this year may look like weight loss, stronger connections in your life, sleeping more, disconnecting from your...
Read More
December Compliance Recap
December was a busy month in the employee benefits world. The U.S. Court of Appeals for the Fifth Circuit held that the Patient Protection and Affordable Care Act’s (ACA’s) individual mandate is unconstitutional. The Internal Revenue Service (IRS) released final instructions and final 1094-B, 1095-B, 1094-C, and 1095-C forms for...
Read More
The NJ Commuter Benefit Law Coming March 2020
The NJ Commuter Benefit Law Coming March 2020 January 10th, 2020 The new year comes with many changes for employers, but it doesn’t just stop after January. With the world constantly changing around us, so are the laws that we must follow. As of March 1st, the New Jersey Commuter...
Read More
The 2020 Leap Year Impacting Payroll
The 2020 Leap Year Impacting Payroll January 9th, 2020 As always, the new year comes with a great deal of changes. With 2020 being a leap year, some of these changes may even be overlooked. A leap year typically occurs every four years, adding one extra day to the month...
Read More
Four Laws That Went into Effect 1/1/2020
There were several notable laws that effect employers beginning 1/1/2020. It is important for employers to understand how these laws effect your employees and business and any necessary next steps you need to take. As always, your Innovative team will help you understand how these changes will affect your plans...
Read More
4 New Year’s Resolutions for an HR Department to Consider
The start of January brings with it the start of a brand-new year, with endless opportunities to be and do better than years past. Often, we consider what goals we would like to set for ourselves personally rather than professionally. Why not set goals for both? Here are a few...
Read More
The ACA’s Cadillac, HIT and Medical Device Taxes Are Repealed; PCORI Fee Extended for 10 More Years
On December 20, 2019, the President signed a $1.4 trillion spending bill that will fund the federal government through September 30, 2020. The bill signed by the President specifically includes the repeal of three major taxes that fund the Affordable Care Act (ACA), including the “Cadillac” tax, the health insurance...
Read More
Myth Series #12: I can’t offer a student loan program in my retirement plan.
With student loan debt reaching astronomical numbers, employers are increasingly looking for ways to add student loan assistance programs to their benefits packages. While current student loan repayment programs can relieve financial stress, they do not offer tax benefits to employees. However, a recent IRS Private Letter Ruling allowing a...
Read More
Broker vs. Fiduciary: The differences you must know
For plan sponsors, running a 401(k) plan can be complex and time-consuming. Some plan sponsors hire outside advisors to help the plan stay compliant with IRS and ERISA laws. It is crucial to understand the difference between hiring a broker versus hiring a fiduciary. Each has a unique set of...
Read More
Adding Wellbeing to Round out your Employee Value Proposition
When it comes to what companies are prioritizing, engagement and wellbeing are now at the top of the list. Many organizations struggle with how to focus on what piece and how much to invest. One thing the research is clear on is that when you combine engagement with wellbeing, you...
Read More
Healthy for the Holidays
The holiday season brings family, friends, festivities and lots of food! The temptations are everywhere and with all the extra activities, your daily routine gets disrupted. How can you stay on track when splurging is so apparent? We can help! Here are a few tips to help keep you healthy...
Read More
November Compliance Recap
November was a busy month in the employee benefits world. The Internal Revenue Service (IRS) released draft 2019 instructions for Forms 1094-B, 1095-B, 1094-C, and 1095-C. The IRS also released health plan limits and various compensation, benefit, and contribution levels under qualified retirement plans for 2020. The Department of Health...
Read More
IRS Extends ACA Reporting Deadline for Furnishing Statements for 2019 from January 31 to March 2, 2020
In Notice 2019-63, the IRS extended the 2020 deadline for employers and insurers to furnish individual statements on 2019 health coverage and full-time employee status (Forms 1095-B and 1095-C) from January 31 to March 2. The notice also extends the good-faith penalty relief to 2019 for incorrect or incomplete reports due in 2020....
Read More
Innovative’s CEO, Terriann Procida, is Awarded “2019 Executive of the Year”
Innovative Benefit Planning is pleased to announce that Terriann Procida has been awarded by South Jersey Biz as one of their 2019 Executive of the Year Award winners! The award recognizes and awards 20 South Jersey professionals who have “paved the way for success.” “As you read through our 2019...
Read More
Required Minimum Distributions
As the calendar year draws to a close, older plan participants may have to consider taking a required minimum distribution (RMD) from their qualified retirement plan. A required minimum distribution is a withdrawal from a qualified retirement plan for participants who have reached the age of 70½. While many qualified...
Read More
Innovative Welcomes Nurse Advocate, Erica Polaneczky, MSN, APRN, ANP-C
We are excited to announce the latest member of the Innovative Benefits team! Please join us in welcoming Erica Polaneczky, MSN, APRN, ANP-C, as our Nurse Advocate. As part of our Workplace Wellness team, Erica will help Innovative build, plan, coordinate, and deliver health promotion activities tailored specifically for each...
Read More
Avoiding and Correcting Common Mistakes on the I-9
Let’s talk about I-9s. You probably filled them out for each employee, filed them away and never thought about them again, right? This can be problematic as there are several common mistakes made on the I-9 form. An audit can be a very costly experience if your forms aren’t all...
Read More
Innovative Welcomes New Director of Wellness & Engagement
We are pleased to announce another new member has joined the Innovative team! Please help us welcome Patricia Pellicore, CWP, as Director of Wellness and Engagement. As Director of Wellness and Engagement Patricia will manage, develop, grow, and promote the numerous positive features of Innovative’s wellness initiatives. One of her...
Read More
Innovative Myth Series #11-As a plan sponsor, I shouldn’t consider adding a 3(16) service to my plan.
An existing client had experienced problems with their 401(k) plan audit for several consecutive years due to internal operational issues. The client requested our help in determining whether they should spend the money for a 3(16) service to help improve efficiencies and eliminate some of the operational errors they were experiencing....
Read More
Innovative’s Well-being @ Work 2019 Summit Recap
As employers, what do we need to create workplaces that are connected, flourishing and well with both business and employee in mind? This year Innovative Benefits Planning hosted our inaugural well-being summit that was dedicated to making workplaces healthier. The room was packed full of HR professionals, C-Suite decision-makers, health...
Read More
Innovative Welcomes Lisa as Director of Compliance
We are excited to announce the latest addition to the Innovative Benefit Planning team! Please join us in welcoming Lisa A. Hill as our Director of Compliance. As Director of Compliance, Lisa will be a valuable resource to Innovative’s leadership team, employees, and clients in ensuring all compliance needs are...
Read More
Diabetes Awareness Month
November is National Diabetes Awareness month! According to the American Diabetes Association, nearly half of all American adults have diabetes or prediabetes, yet most do not fully understand the illness. Unaddressed diabetes can take a heavy toll medically, financially, and personally. Diabetes also increases the risk of developing other chronic...
Read More
Innovative Benefit Planning Earns Specialized Advisor Recognition
Our firm was founded on the principles of integrity, professionalism and exceptional client service. We are also deeply committed to continuous improvement. Our dedication to doing what is best for you, our clients, prompted us to engage CEFEX, the Centre for Fiduciary Excellence, LLC to audit our processes. In June...
Read More
2020 IRS Contribution Limits Released
On Wednesday, the IRS announced new contribution limits for medical FSA, Commuter Benefit, and HSA plans for 2020. The FSA contribution will increase to $2,750, a $50 increase from current limits. The HSA contribution limit for individuals with a high deductible health plan (HDHP) will likewise be raised from $3,500...
Read More
October Compliance Recap
Compliance Recap-October 2019 October was a relatively quiet month in the employee benefits world. The U.S. District Court for the Northern District of Texas vacated portions of the current rule implementing Section 1557 that prohibit discrimination on the basis of gender identity and pregnancy termination. The U.S. Court of Appeals...
Read More
Innovative Myth Series #10: When Transferring Service Providers, There are no Pitfalls, Part 2 – Market Value Adjustments and Fixed Accounts
A new client engaged Innovative after they decided to transfer their current plan to a new service provider. After our initial investment review, we noticed there was an existing Stable Value Fund, which was subject to a market value adjustment (MVA). When an MVA is being applied, a complete fund...
Read More
Should you Consider a Safe Harbor Contribution Feature?
Does your organization’s retirement plan frequently refund money to highly compensated employees (HCE)? Do you want to provide a great incentive to your employees to save for retirement and perhaps allow them to retire earlier? Would the owners and highly compensated employees like to save more of their own money?...
Read More
Diversity Discussion: Terms to Know
The concept of diversity is often presented to employees only in the negative – employees are told not to discriminate, or not to harass. But diversity is much more than that – when embraced and fostered, it promotes creative, engaged, happy workplaces. Beginning the diversity discussion with your workforce can...
Read More
Ryan Kastner Receives Young Professionals Leadership Award
Congratulations to our Vice President, Consulting, Ryan Kastner, for being named to Burlington County Regional Chamber of Commerce’s (“BCRCC”) Young Professionals Leadership Class of 2019. The award honors professionals under the age of 40 who demonstrate outstanding leadership in the Burlington County Business Community. Winners are selected based on their...
Read More
Oral Health Awareness Month
Did you know that your oral health offers clues about your overall health — or that problems in your mouth can affect the rest of your body? Protect yourself by learning more about the connection between your oral health and overall health. What’s the connection between oral health and overall...
Read More
September 2019 Compliance Recap
September was a busy month in the employee benefits world. The U.S. Senate confirmed Eugene Scalia as the new Secretary of the Department of Labor (DOL). The Internal Revenue Service (IRS) published proposed rules regarding affordability safe harbors and Section 105(h) nondiscrimination rules as applied to individual coverage health reimbursement...
Read More
DOL Overtime Rule Change
On Sept 24th, the US Department of Labor (DOL) released a new rule, increasing the minimum salary level for exempt status to $35,568 per year for a full-time employee, effective January 1, 2020. Read the full law, here: DOL Overtime Rule Change The proposed rule creates the...
Read More
9 Employee Handbook Essentials
There are so many things that are essential to the employee handbook that it can be tough to know where to even start. We’ve got you covered. Below are 9 key components that every good employee handbook should include. 1. Introductory Statement This statement introduces the handbook, describes the purpose...
Read More
5 Reasons To Hire the Right Financial Advisor For Your Retirement Plan
As an organization offering a retirement plan to their employees, plan sponsors are faced with decisions that can affect the entire organization. The plan design, investment line-up, and who the recordkeeper will be are typical for all plans. Beyond these standard decisions, there is the issue of knowing and understanding...
Read More
30 Years and 30 Reasons to Choose Innovative
When it comes to benefits planning, there are a ton of choices out there. And, we believe we’re the most innovative company you’ll find. After 30 years, here are 30 good reasons our clients choose to work with us: We put people first We are an advocate for our clients...
Read More
Innovative Myth Series #9: When Transferring Service Providers, There Are No Pitfalls. Part 1-Protected Benefits
A new client engaged Innovative to transfer their current plan to a new service provider. During the course of our detailed review, we discovered that certain employees had annuity contracts with death benefits that exceeded the value of their plan investments. If the client executed the transfer, these participants would...
Read More
Flu Season: Myths vs. Facts
Flu season is quickly approaching. The Centers for Disease Control and Prevention (CDC) recommends that those aged 6 months and older receive the flu vaccine by the end of October. Getting a flu vaccine is the first and most important step in protecting against the flu. There are many misconceptions...
Read More
August 2019 Compliance Recap
August was a relatively quiet month in the employee benefits world. The Department of Labor (DOL) issued its updated Medicaid / CHIP Model Notice. The Centers for Medicare and Medicaid Services (CMS) revised its Medicare Secondary Payer User Guide and changed reporting requirements regarding prescription drug coverage beginning January 1,...
Read More
Innovative Celebrates 30 Year Anniversary
Before 2019 came to an end, Innovative Benefit Planning had to officially celebrate our 30 Year anniversary, and we certainly didn’t get here alone. On July 24th, our employees, partners and clients, came together to enjoy food trucks, music, and memories from over the years. The afternoon was filled with...
Read More
Innovative Benefit Planning Named “Best of Biz 2019”
Innovative Benefit Planning has been named by South Jersey Biz, as one of their 2019 Best of Biz recipients. The Best of Biz award recognizes 102 of region’s most esteemed service providers and we are proud to say that Innovative has been selected for their “Employee Benefits” category. According to...
Read More
Do’s and Don’ts When Creating an Employee Handbook
The employee handbook is an important communication resource for your employees that also limits your company’s legal liability. It can be tough to decide what does and does not belong in the employee handbook, but these tips can help you along the way. Read the full article, here.
Read More
Vice President, Consulting, Dan Foley, Named to Rand Institute Advisory Board at Rutgers University–Camden
The Senator Walter Rand Institute for Public Affairs at Rutgers University–Camden, an institute for public policy issues impacting southern New Jersey, announced last week that Innovative’s Vice President, Consulting, Dan Foley, has been appointed to their advisory board. Dan is joined by two other regional leaders, Amy Obsorn, vice president...
Read More
Innovative Myth Series #8: Once I Sell a Company, I Don’t Have To Worry About It Impacting My Current Retirement Plan
See how Innovative helped our client from running afoul of the Affiliated Service group rules and saved the client from potential serious regulation issues. Let Innovative perform a complimentary review of your plan, contact our retirement planning team here.
Read More
Mind Your Health-Mental Health & Exercise
You have probably heard of the variety of benefits from weekly exercise…. But did you know that exercise can do wonders for both physical AND mental health? People who exercise regularly gain a sense of well-being, feel more energetic throughout the day, have a better quality of sleep, and have...
Read More
NJ Bans Salary History
On July 25th, 2019, New Jersey’s Acting Governor Sheila Oliver signed NJ Bill A1094 (“the Law”), which bans employers from asking applicants for their salary history. Read the full law here, NJ Bans Salary History, to learn: What is now illegal for an employer to do What the law allows...
Read More
July 2019 Compliance Recap
July was a busy month in the employee benefits world. The Internal Revenue Service (IRS) released a notice that expands the list of preventive care benefits a high deductible health plan can provide without a deductible or with a deductible below the annual minimum deductible. The IRS also released the...
Read More
Additional Preventive Care Benefits Permitted for High Deductible Plans
In Executive Order 13877, issued June 2019, the Treasury Department and the IRS were directed to consider ways to expand the use and flexibility of HSA’s and HDHP’s. In response to the Executive Order, the Treasury Department issued guidance on July 17, 2019, that lists newly identified preventive care items...
Read More
Cybersecurity: The Need for Both IT and HR
Businesses face a multitude of risks throughout their daily operations. One of the most complicated risks that organizations confront is cybersecurity risk. Cybersecurity is defined as the protection of internet-connected systems, including hardware, software and cyberattacks. When businesses hold sensitive data on the cloud or shared servers, you must address...
Read More
Pennsylvania Medical Marijuana Updates
Effective July 20, 2019, Pennsylvania will recognize anxiety and Tourette Syndrome as serious medical conditions in the medical marijuana program. The Pennsylvania Department of Health stated that the decision came after a research-based recommendation by the state’s Medical Marijuana Advisory Board, followed by Health Secretary Rachel Levine ’s careful review of the...
Read More
Innovative Myth Series #7: The Only Benefit To A Retirement Plan is Retirement Savings
See how Innovative helped this client add a pension plan to their existing 401(k) and profit-sharing plan offerings to tackle their recruiting and retention challenge. Download full case study here. Let Innovative perform a complimentary review of your plan, contact our retirement planning team here.
Read More
HRA Final Rules
The Department of the Treasury (Treasury), Department of Labor (DOL), and Department of Health and Human Services (HHS) (collectively, the Departments) recently released their final rules regarding health reimbursement arrangements (HRAs) and other account-based group health plans. An HRA is a type of account-based group health plan funded solely by...
Read More
Four Tips for Managing Five Generations in One Workplace
As organizations become more age diverse, business leaders find themselves managing a multigenerational workforce. Five generations in the workplace can mean more opportunity for success or more challenges, depending on how an organization deals with the generational differences. Each generation has grown up in very specific times in history and...
Read More
EEOC Component 2 Data Update
On July 2, 2019, following initial notifications to employers of the upcoming Component 2 filing deadline, the EEOC updated the Component 2 website to include both Additional Information https://eeoccomp2.norc.org/info.html and Frequently Asked Questions (FAQs) sections. https://eeoccomp2.norc.org/faq.html Under the Additional Information section, employers can find a sample form, an instruction booklet,...
Read More
Do you Practice Sun Safety?
Summer is here! That means spending more time with the family, more outdoor activities, and most importantly more exposure to the sun and its harsh UV rays. Increased exposure to UV radiation increases the risk of skin cancer. Due to climate change, the stratospheric ozone is thinning allowing less protection...
Read More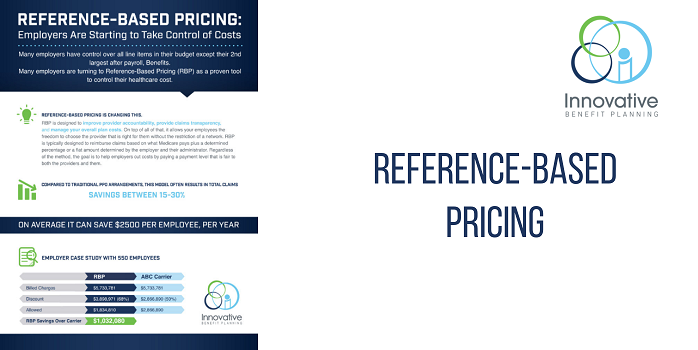
Reference-Based Pricing: Employers Are Starting to Take Control of Costs
You may have heard of Reference-Based Pricing as the healthcare strategy gains momentum to control healthcare costs. But what is it and how does it work? Click below to learn what Reference-Based Pricing is and the pros and cons to consider. Innovative’s unique Reference-Based Pricing 6 step process first makes...
Read More
President Trump Signs an Executive Order to Improve Price and Quality Transparency in Healthcare
President Trump signed an executive order directing federal agencies to increase healthcare price and quality transparency. The order specifically directs the Departments of Labor, Treasury and Health and Human Services to issue guidance and propose regulations that would disclose negotiated rates, cost-of-care and de-identified federal healthcare data, and to expand...
Read More
NJ Now Has Greater Protections for Employees Who Are Cannabis Users
On July 2, 2019, New Jersey Governor Phil Murphy signed a bill into effect that overhauls the state’s existing medical cannabis program and law, the Compassionate Use of Medical Marijuana Act (CUMMA), and greatly expands patient access to medical marijuana. For employers who must address the issue of employees and...
Read More
June 2019 Compliance Recap
June was a relatively busy month in the employee benefits world. The Department of Labor (DOL), the Department of Health and Human Services (HHS), and the Department of Treasury published final rules that removed the prohibition against integrating a health reimbursement arrangement (HRA) with individual health insurance coverage and recognized certain...
Read More
Innovative Myth Series #6: Funding a Profit Sharing Plan for a Company with More Than 100 Employees Will Only Benefit My Employees
See how Innovative helped one client generate significant tax savings for their company. Download full case studyhere. Let Innovative perform a complimentary review of your plan, contact our retirement planning team here. Download full case...
Read More
HHS Proposes to Revise ACA Section 1557 Rule
On May 24, 2019, the Department of Health and Human Services’ Office for Civil Rights (OCR) released a proposed rule to revise its regulations under the Patient Protection and Affordable Care Act’s Section 1557. OCR also released a fact sheet and press release. The proposed rule would eliminate: Certain definitions,...
Read More
Andrew Gloninger Joins as Benefits Guardian
It gives us great pleasure in introducing our newest member, Andrew Gloninger, to the Innovative team! Andrew joins Innovative’s employee benefits department as a Benefits Guardian. This position is a key member of the client services team and will serve as a direct point of contact for our client’s employees....
Read More
Kyra Foster Joins as HR and Recruiting Coordinator
We are excited to welcome our newest member of the Innovative team. Please join us in welcoming Kyra Foster as HR and Recruiting Coordinator. In this position, Kyra is responsible for assisting with all internal and external HR related inquiries or requests, as well as providing support to the VP...
Read More
The Importance of a Roth Option in Retirement Plans
Roth contributions can provide significant benefits to retirement plans for both participants and plan sponsors alike. But what does Roth mean? Unlike pre-tax, Roth refers to post-tax dollars, meaning the money has already been taxed when it goes into a participant’s account. They are beneficial to participants because qualified Roth...
Read More
Self-Care for Caregivers
National Women’s Health Week was May 12-18 this year. Earlier this month, we focused on preventative health, by age, for women. But a large percentage of women fall into a different type of health risk category–being a caregiver for a friend or family member. Besides physical health, caregivers also need...
Read More
National Women’s Health Week
The 20th annual National Women’s Health Week kicked off this past Sunday on Mother’s Day, May 12, and is celebrated through May 18. Each year, this week serves as a reminder for women to make their health a priority and build positive health habits for life. What steps can you...
Read More
Migraine and Headache Awareness Month-How to Cope in the Workplace
Almost 40 million Americans live with migraine and headache disorders. Unfortunately, headaches are considered invisible diseases, due to its ability to cause people who live with it to feel isolated and alone. There is a lack of understanding from employers, the public and people with migraine themselves about the impact...
Read More
May 2019 Compliance Recap
May was a busy month in the employee benefits world. The Internal Revenue Service (IRS) released health savings account annual contribution limits and high deductible health plan minimum annual deductibles and annual out-of-pocket maximums for 2020. The Department of Labor (DOL) released questions and answers (Q&As) to clarify its enforcement...
Read More
June is Men’s Health Month
Men’s Health Month is celebrated across the country during the month of June with screenings, health fairs, media appearances, and other health education and outreach activities. The purpose of Men’s Health Month is to heighten the awareness of preventable health problems and encourage early detection and treatment of disease among...
Read More
Innovative Myth Series #5: Plans With No Financial Consultant Receive The Best Fees And Fiduciary Protection From Their Qualified Plan Provider
See how Innovative’s experience with reviewing “Retirement Plan Relationships” helped one client in negotiating lower administrative fees, increased services for the plan sponsor and streamlined administrative functions. Download full case study here. Let Innovative perform a complimentary review of your plan, contact our retirement planning team here.
Read More
HR Person of the Year Awards Dinner
Last week, Innovative attended the 19th Annual Delaware Valley HR Person of the Year Awards Dinner as a proud Silver Sponsor. Our very own Ryan Kastner was nominated as HR Consultant of the Year! A lovely time was had by all. It was truly a successful event, raising $9,290 to benefit...
Read More
EEOC Pay Data Collection
The Equal Employment Opportunity Commission (“EEOC”) announced that it will collect information from applicable employers on employee pay and hours-worked—known as Component 2 data—for 2017 and 2018 as part of the annual EEO-1 report and the data is due by September 30, 2019. The Department of Justice filed a Notice...
Read More
Compliance Alert: IRS Raises HSA/HDHP Limits for 2020
Compliance Alert: IRS Raises HSA/HDHP limits for 2020 The IRS has announced that effective January 1, 2020, an individual in a High Deductible Health Plan (“HDHP”) with self-only coverage has a new maximum allowable annual contribution into a Health Savings Account of $3,550 , increased from $3,500. The maximum annual...
Read More
Colette Crosby Joins as Account Manager
As Innovative continues to grow, we are excited to announce another new member to the Innovative team. Please join us in welcoming Colette Crosby as Account Manager. Colette will be reporting to the Account Executives Elizabeth Ferroni and Shemelia McClain. As Account Manager, Colette will be responsible for supporting the...
Read More
Benefits to Offering a 401(k) plan
According to the recent Jobvite’s Recruiter Nation Survey, after Healthcare, 401(k)s are considered the most valuable benefit to recruit and retain employees. Providing retirement benefits to your employees, such as 401(k) plans, is an important step in recruiting, retaining and promoting employee wellness. Recruitment and retention: Recent trends demonstrate...
Read More
Are Target Date Funds Right for Your Participants?
In recent years, plan sponsors have increased the inclusion of Target Date Retirement funds in their investment fund lineup. In fact, J.P. Morgan estimates that 88% of new retirement plan contributions are expected to flow into Target Date Funds by end of this year1. Here are some of the reasons...
Read More
April 2019 Compliance Recap
April was a busy month in the employee benefits world. The Centers for Medicare & Medicare Services (CMS) issued its parameters for the defined standard Medicare Part D prescription drug benefit for 2020. In the court case challenging the Patient Protection and Affordable Care Act’s constitutionality, the court will hear...
Read More
Andrew May Earns Accredited Investment Fiduciary Designation
Innovative is proud to announce that Andrew May has been awarded the Accredited Investment Fiduciary designation from the Center for Fiduciary Studies, the standards-setting body for fi360. Andrew is a Financial Services Associate working in the retirement services department. He is responsible for servicing the firm’s qualified plan clients in...
Read More
A Nutrition Approach to Prostate Cancer Prevention
According to the American Cancer Society, one in six men will be diagnosed with prostate cancer in his lifetime. Prostate cancer is a disease in which some of the cells of the prostate gland grow and divide in an uncontrolled way. The resulting mass is called a malignant tumor, which...
Read More
New NJ Commuter Law
Governor Murphy signed a new law on March 1, 2019, read here: Commuter Law, requiring certain employers to provide pre-tax commuter fringe benefits to employees. New Jersey employers with at least 20 employees in the state will need to begin offering those employees pre-tax transportation fringe benefits covering commuter highway vehicle...
Read More
March 2019 Compliance Recap
March was a busy month in the employee benefits world. The Department of Justice (DOJ) announced that it will not defend the Patient Protection and Affordable Care Act (ACA) in the court case challenging the ACA’s constitutionality. The Internal Revenue Service (IRS) updated two Q&As regarding ACA reporting for 2018....
Read More
Innovative Welcomes Eileen Green as Chief Operating Officer
Innovative is proud to announce that industry executive leader, Eileen Green, has joined Innovative as Chief Operating Officer. Reporting directly to our CEO, Terriann Procida, this key new position will be integral to ensuring that Innovative has the proper operational controls, administrative and reporting procedures to provide operational excellence across...
Read More
Innovative Myth Series #4 Employer Profit-Sharing Deductions Must Be Recognized in the Year the Contribution is Made
See how Innovative’s strategic planning and Profit-Sharing experience helped our client maximize tax benefits and fund significant plan contributions for their key employees. Download full case study here. Let Innovative perform a complimentary review of your plan, contact our retirement planning team here.
Read More
Innovative is Awarded the “Community Impact Award”
Innovative Benefit Planning is honored to announce we are the recipient of the “Community Impact Award”. Issued by the South Jersey Biz, Innovative is featured as one of the inaugural winners in their April 2019 publication. The award honors successful companies in South Jersey that, in addition to their business...
Read More
Innovative Celebrates National Pet Day at Burlington County Animal Shelter
To celebrate our 30-year anniversary and pay thanks to our amazing community and countless partners, Innovative has pledged to give back in 30 ways this year. We are dedicated to making our community a key part of our business in 2019. From local charities and non-profits to those in need...
Read More
Allergy Prevention Tips
Did you know that you can sign up for allergy alerts? You will get email notifications of allergy counts in your area. On days that the pollen count is high, avoid leaving windows to your home and car open. Pollen counts are the highest between the hours of 5am-10am. If...
Read More
Spring Has Sprung! But So Has Allergy Season
Spring has sprung! But so has allergy season According to the Asthma and Allergy Foundation of America, allergies are classified as a chronic disease. So, what are allergies? An allergic reaction occurs when the body’s immune system treats an allergen such as pollen, as a harmful substance. The immune system...
Read More
Innovative Welcomes Brooke Haramija as Marketing Coordinator
Brooke Haramija joins the Innovative team as Marketing Coordinator, reporting directly to Jamie Bratton, Director of Marketing & Communications. Brooke will be responsible for helping to create and implement marketing strategies for all Innovative’s products and services, by developing and implementing marketing and advertising campaigns. In addition, she will help...
Read More
Innovative Myth Series #3: Mergers and Acquisitions are Simple
Innovative’s merger and divestiture of plans consulting expertise enabled us to provide complete end -to-end service. See how we helped our client ease their administrative burden and reduce client fees by over 40%. Let Innovative perform a complimentary review of your plan, contact our retirement planning team here.
Read More
Innovative Welcomes Andrew May as Financial Services Associate
We are excited to announce our newest member of the Innovative team, Andrew May. Andrew joins the firm as a Financial Services Associate. In this role, Andrew will work with the Retirement Consulting Division and be responsible for servicing the firm’s qualified plan clients. His duties will also include participant...
Read More
February 2019 Compliance Recap
February was a quiet month in the employee benefits world. The Internal Revenue Service (IRS) released an information letter addressing when an employer may seek recoupment of contributions made to an employee’s HSA. A U.S. District Court held that the State of Maryland could not ask for a declaration that...
Read More
Action-Based Wellness-How it Can Reduce Claims Cost 10-25%
See how Innovative helped one client save significant claims dollars over a three year period by implementing a “results-based” wellness program. During the three year period, Innovative was able to help our client: Obtain 96% of employees to participate in Biometric Screenings Implement a proactive outreach incentive program 60% of employees to improve or remain low...
Read More
Recent Updates in New Jersey Law
A lot has been happening in New Jersey since the new year began, and there have been a few critical updates for New Jersey employers and employees. New Jersey Minimum Wage On January 17, 2019, Governor Phil Murphy and legislative leaders agreed on legislation that will incrementally increase New Jersey’s...
Read More
Innovative Welcomes Rbhya Pal as Actuarial Analyst
It gives us great pleasure in introducing our newest member, Rbhya Pal, to the Innovative team! Rbhya joins Innovative’s employee benefits department as an Actuarial Analyst, reporting to our Director of Benefits Consulting, John Romaska. Rbhya will be responsible for preparing client claims reports and analysis, marketing various funding arrangements...
Read More
Ryan Kastner Nominated for HR Consultant of the Year
Congrats to our very own Ryan Kastner on his nomination for this year’s HR Consultant of the Year! The Delaware Valley HR Person of the Year Award was developed in 2001 to celebrate the Human Resources industry and to recognize those in the HR profession who exemplify outstanding achievement within...
Read More
National Nutrition Month
National Nutrition Month® is an annual campaign started by the Academy of Nutrition and Dietetics to raise awareness of the importance of making informed, healthful food choices to prevent and combat illness. Did you know that food is the most powerful medicine? Medicine comes with many positive and negative effects...
Read More
Innovative Attends NAHU Capitol Conference
February 24-27th, Vice President Consulting Ryan Kastner, Director of Marketing Jamie Bratton and Vice President of HR & General Counsel, Deirdre Groenen, Esq. attended the 2019 NAHU Capitol Conference in Washington, DC. During their time in Washington, the trio attended three days of informative sessions that detailed changing legislation that...
Read More
January 2019 Compliance Recap
January was a relatively quiet month in the employee benefits world. The Department of Labor (DOL) issued its annual adjustment of federal civil monetary penalties. The Centers for Medicare & Medicaid Services released a proposed rule for benefit payment and parameters for 2020. The Internal Revenue Service (IRS) released its...
Read More
Innovative Myth Series #2: All Highly Compensated Employees are Defined by Salary Alone
See how Innovative’s experience with qualified plans helped this client to be compliant with ADP testing. Download full case study here. Let Innovative perform a complimentary review of your plan, contact our retirement planning team here.
Read More
Innovative Pledges 30 Givebacks for 30 Years
To celebrate our 30-year anniversary and pay thanks to our amazing community and countless partners, Innovative has pledged to give back in 30 ways this year. We are dedicated to making our community a key part of our business in 2019. From local charities and non-profits to those in need...
Read More
Gen Z is Coming. Is Your Workplace Ready?
While it may feel like businesses are still reeling from adapting to the working millennial, the next generation is already knocking on the HR door. The Society for Human Resource Management went straight to a 16-year old source to see what is on the workplace horizon. Here are a few trends...
Read More
Innovative Myth Series #1: I Can Rely on My Recordkeeper to Manage Terminated Employees
See how Innovative’s experience with retirement plans helped this client find substantial savings by examining their 401(k) plan. Download full case study here. Let Innovative perform a complimentary review of your plan, contact our retirement planning team here.
Read More
December Compliance Recap
December was a relatively quiet month in the employee benefits world. A U.S. District Court issued an order declaring that the Patient Protection and Affordable Care Act (ACA) is unconstitutional. The Equal Employment Opportunity Commission (EEOC) issued two final rules to remove certain wellness program incentives. The Department of Labor...
Read More
Workplace Wellness Tips to Fend off the Flu
It’s that time of year again, when we start to hear coughing, sniffling and sneezing around the office and everyone starts to panic because no one wants to get sick, especially with the flu! When is flu season? Flu season begins in October and ends as late as May, however...
Read More
10 FAQs Regarding The New Jersey Paid Sick Leave Act
1.) Earned sick leave may be used for: The treatment, care or diagnosis for employee or family member Employee or family member a victim of domestic or sexual violence (*has no 25 employees + or 1,000 hours worked requirement like the NJ Safe Act). Workplace or school/daycare closed by a public...
Read More
Is Your Workplace Wellness Program Compliant?
In a recent settlement, the Department of Labor (DOL) imposed over $160,000 in fines and penalties on an employer for the noncompliant tobacco surcharge they imposed through their plan’s Wellness Program. A common Wellness Program design is to impose a premium surcharge to employees who use tobacco products. This surcharge...
Read More
New Year, Fresh Start
2019 is in full swing and it’s the time of year that we get to designate as a fresh start and new beginnings. It’s a tradition in which we resolve to change an undesired trait or behavior, to accomplish a personal goal or otherwise improve our health and life in...
Read More
Innovative Welcomes Shemelia McClain as Executive Account Manager
Innovative Benefit Planning is excited to welcome Shemelia McClain as our new employee benefit Executive Account Manager. Shemelia brings to Innovative more than 20 years of experience as an account manager and leader in the employee benefits industry. In her new role as Executive Account Manager, Shemelia will be responsible...
Read More
The IRS Increases the PCORI Fee
The Internal Revenue Service announced that the Patient-Centered Outcomes Research Institute (PCORI) fee will rise to $2.45 (from $2.39) per covered life in plan years that fall between October 1, 2018, and September 30, 2019. This increase will have an impact on 2019 plan year rates and is attributable to...
Read More
Tax Credit Check from Horizon
Attention Horizon customers! You may have received or will receive shortly, a check in the mail from Horizon regarding a tax credit refund check. Note, this is a legitimate check and you can use these funds however you see fit. Why are you receiving this check? In late 2017, the...
Read More
Retirement Match on Student Loan Debt- UPDATE
In October we reported on a Private Letter Ruling the IRS issued for an employer interested in offering a student loan repayment benefit through their 401(k) plan. While the ruling only applied to the plan and plan sponsor who requested it, we suspected at the time that the ruling would...
Read More
November Compliance Recap
November was a busy month in the employee benefits world. The Internal Revenue Service (IRS) extended the due date for employers to furnish Forms 1095-C or 1095-B to individuals, extended “good faith compliance efforts” relief for 2018, and issued specifications for employer-provided substitute ACA forms. The Department of the Treasury...
Read More
Let’s Discuss Tax Relief from Your 199A Deduction
Earlier this week we discussed the Tax Cuts and Jobs Act of 2017 and the limits placed on the deductibility of State and Local taxes for 2018. Now let’s discuss your 199A deduction. For many owners of pass-through entities, _ the new 199A deduction will generate welcome tax relief in...
Read More
There May Be a Simple Solution to Decrease the 2018 Tax Burden Through a Customized Retirement Plan Design
The Tax Cuts and Jobs Act of 2017 have limited the deductibility of State and Local taxes for 2018. As a result, many high earners may be subject to additional taxes this year. However, there may be a simple solution to decrease the 2018 tax burden through a customized retirement...
Read More
Happier Holidays, the HR Way
Most people, according to a new survey featured in HR Dive, have the greatest sense of belonging in their own homes. That may not be surprising news, but what is interesting is that one-third of respondents felt the greatest sense of belonging in their workplace. A significant percentage, 40 percent, attribute...
Read More
ACA Extensions Announced
Yesterday afternoon, the IRS released Notice 2018-94, which announced an extension of the 2019 deadline for insurers and employers to furnish forms 1095-B and 1095-C to individuals. These forms, originally due January 31, 2019 are now due March 4, 2019. Although the furnishing deadline has been extended, the IRS has...
Read More
Innovative Welcomes Mercedes Gutierrez, MD as Director of Wellness and Population Health Services
We are excited to announce another new member to the Innovative team! Please join us in welcoming Mercedes Gutierrez, MD, as Director of Wellness and Population Health Services. As Director of Wellness and Population Health Services, Mercedes will be responsible for managing, growing, and promoting the many positive aspects of...
Read More
Innovative Compliance- The New Jersey Equal Pay Act
As of July 1, 2018, the Diane B. Allen Equal Pay Act (“the Act”), which amends the New Jersey Law Against Discrimination (“LAD”), went into effect in New Jersey. The Act applies to all New Jersey public and private employers regardless of size, except federal employers. https://www.njleg.state.nj.us/2018/Bills/S0500/104_R2.PDF Pursuant to the...
Read More
New Tri-Agency Proposed Rule on Health Reimbursement Arrangements
The Department of the Treasury (Treasury), Department of Labor (DOL), and Department of Health and Human Services (HHS) (collectively, the Departments) released their proposed rule regarding health reimbursement arrangements (HRAs) and other account-based group health plans. The DOL also issued a news release and fact sheet on the proposed rule....
Read More
Important NJ Earned Sick Leave Update
In yesterday’s blog post, we discussed the New Jersey Earned Sick Leave Law, which went into effect this Monday, October 29th. For more on the specifics of the law. In addition to the employer obligations outlined in the previous post, all employers with employees working in New Jersey must post...
Read More
The Benefits of Seasonal Produce
You always hear about the importance of eating fruits and vegetables. Indeed, they are packed with vitamins, minerals, fiber, and other phytonutrients that are beneficial to our health! But did you know that eating seasonal produce is not only higher in nutrients, but also cheaper, better tasting, and more environmentally-friendly?!...
Read More
NJ Earned Sick Leave Law Goes into Effect
For New Jersey employers (or PA, NY or other employers who have employees who work in NJ), the NJ Earned Sick Leave Law went into effect Monday, October 29, 2018. Below is a link to a very comprehensive list of FAQs on the law, but here are some highlights: There...
Read More
Innovative Supports Oaks Integrated Care at the Moorestown Progressive Dinner
Friday, October 19th, Terriann Procida, Mark Sulpizio, Jamie Bratton, and Ryan Kastner represented Innovative at the Oak Integrated Care 14th Annual Moorestown Progressive Dinner. Each year, ten homes in Moorestown host a small group of guests for a delicious dinner prepared by a local chef. This year’s chefs came from...
Read More
Innovative Announces new VP of HR and General Counsel
Please join us in welcoming Deirdre Groenen, Esq. as VP of HR and General Counsel__. Reporting directly to our CEO, Terriann Procida, this new key member of the senior leadership team will provide guidance, conduct research, and serve as a resource for our employees and our clients. This role is...
Read More
Innovative Shows Support of Samaritan Healthcare and Hospice at Memorial Paver Reveal
This Tuesday, Innovative Principal, Mark Sulpizio, attended an Open House at the Samaritan Center at Voorhees where Samaritan Healthcare and Hospice revealed the first of their memorial pavers. The memorial pavers are a beautiful way to memorialize loved ones and border the walkways of the gardens at Samaritan’s new Voorhees...
Read More
Innovative Welcomes Jamie Bratton as Director of Development & Communications
Jamie Bratton joins Innovative’s marketing department as Director of Development & Communications. Reporting to our CEO, Terriann Procida, this position is responsible for establishing and implementing strategic and tactical communication plans across every Innovative business unit, designed to capitalize on market opportunities, generate demand of Innovative’s services and help to...
Read More
Student Loan Considerations for Plan Sponsors-Part Two
As a follow up to our first article on student loan debt, its impact on employers and the recent IRS Private Letter Ruling (PLR) regarding student loan repayments, we’ve attached a summary of items to consider when contemplating this type of arrangement. As this ruling has just been released, we...
Read More
Innovative’s Ryan Kastner Appointed Local United Way Campaign Cabinet Chair & Voted to Become County Board Member
Innovative Benefit Planning is pleased to announce that Vice President, Consulting, Ryan Kastner has been appointed as United Way of Greater Philadelphia and Southern New Jersey’s Campaign Cabinet chair for 2018-2019. As Campaign Cabinet Chair, Ryan’s role will assist in facilitating the United Way’s mission by working with CEOs and...
Read More
IRS Allows 401K Match for Student Loan Repayments
The IRS recently issued a Private Letter Ruling (PLR) for an employer interested in offering a student loan repayment benefit through their 401(k) plan. While the ruling only applies to the plan and plan sponsor who requested it, the ruling will most likely expand interest in this type of program,...
Read More
Innovative CEO, Terriann Procida, Receives Mid-Atlantic Women’s Leadership Award
Last night at the Downtown Club in Philadelphia, PA, Innovative Benefit Planning’s CEO, Terriann Procida, was one of 50 women to be recognized by CEO Report as one of their 2018 Mid-Atlantic Women’s Leadership Award winners. The Women’s Leadership Awards program honors CEOs and Executives who are moving their companies...
Read More
A Hard Habit to Break
Smoking is an addiction and as most smokers know, quitting isn’t easy. Quitting smoking is a journey, not a single event. You might hit some bumps in the road during your journey to quit smoking. Having a plan to meet these challenges is an important part of quitting for good....
Read More
Ryan Kastner Promoted to Vice President, Consulting
Innovative Benefit Planning is pleased to announce the promotion of Ryan Kastner to Vice President, Consulting. Ryan has been with Innovative for almost 6 years as Employee Benefits Consultant and like his prior role, Ryan will continue to consult with clients on their benefit and retirement plans and identify key...
Read More
Are Your Retirement Plan Committee Members Aware of Their Fiduciary Obligations?
Do your retirement plan committee members have a thorough understanding of their fiduciary obligations? In a recent court case involving the retirement plans offered at New York University, the court found that certain committee members were not fully aware of their obligations as Fiduciaries. At Innovative Benefit Planning, we assist...
Read More
The Benefits of Positive Thinking
Many people do not know that positive thinking has a lot of health benefits. If you keep your mind in good shape, you’ll have an optimistic view of life and that affects your health and wellbeing in an extremely positive way. On the same note, thinking negatively can have an...
Read More
Dan Foley Promoted to Vice President, Consulting
Innovative Benefit Planning is proud to announce that Dan Foley has recently been promoted to Vice President, Consulting. Like his prior role as Employee Benefits Consultant, Dan will continue to consult with clients on their benefit and retirement plans and identify business development opportunities. As part of the leadership team,...
Read More
Wellness Team Earn Their Certified Corporate Wellness Specialist® Designation
Congrats to our Worksite Wellness Coordinator, Erica Brown and our Project Manager, Kim Fisher on earning their Certified Corporate Wellness Specialist® designation. The Certified Corporate Wellness Specialist® is the foremost designation available in the corporate wellness and well-being field. The CCWS course comprises of concise and comprehensive techniques in how...
Read More
Terriann Procida is Awarded “2018 Women’s Leadership Award”
Innovative Benefit Planning is pleased to announce that Terriann Procida has been awarded by CEO Report as one of their 2018 Mid-Atlantic Women’s Leadership Award winners! The award recognizes and awards CEOs who are growing and “moving their companies forward.” “This year’s Mid-Atlantic Women’s Leadership Awards winners have made outstanding...
Read More
Vincent Madle, Innovative Summer Intern, Officially Joins Innovative Team
Please join us on congratulating our summer intern, Vincent Madle, as he finished his last day as intern on August 28th! Vincent is entering his last year at Temple University in their Risk Management & Insurance Program. During his time here, he has been an immense resource to our team,...
Read More
Innovative’s Executive Account Manager, Elizabeth Ferroni, attends Annual Employee Benefits Symposium
Our Executive Account Manager, Elizabeth Ferroni, just came back today from attending the Annual ISCEBS Employee Benefits Symposium in Boston, MA. Now in its 37th year, the symposium brings together thousands of benefit professionals to learn, discuss and hear from industry experts and leaders. Elizabeth is excited to be back...
Read More
NJ Consumer Protection Act goes into effect on August 29, 2018
On August 29th, 2018, the “Out-of-network Consumer Protection, Transparency, Cost Containment and Accountability Act” will go into effect. All fully-insured health plans must follow the New Jersey state mandate, while self-funded health plans can decide to opt-in. Innovative Benefit Planning has prepared a brief on what employers should know about...
Read More
June Compliance Recap
June was a relatively quiet month in the employee benefits world. The U.S. Department of Labor issued final regulations regarding association health plans. The U.S. Department of Justice filed a response in ongoing litigation regarding the constitutionality of the Patient Protection and Affordable Care Act. The Centers for Medicare and...
Read More
Elizabeth Ferroni Promoted to Executive Account Manager
Innovative is proud to announce that Elizabeth Ferroni has been promoted from Account Manager to Executive Account Manager. Elizabeth has been an invaluable resource to the Innovative team and to our clients and is well deserving of this new title. As an Executive Account Manager, Elizabeth will maintain the ability...
Read More
Trump Administration Suspends Billions in Risk Adjustment Payments to Insurers
Background The implementation of the Affordable Care Act brought uncertainty to many insurers. To guard against adverse selection, and the threat of insurer insolvencies, the federal government enacted safety measures to stabilize the individual markets. The “3 R’s of Health Insurance” sought to balance the risk pool by eliminating uncertainty...
Read More
Innovative Welcomes Vincent Madle
We are excited to welcome our summer intern, Vincent Madle, to the Innovative team! Vincent is a rising senior at the Temple Fox School of Business and is currently pursuing a BBA in Risk Management & Insurance with a concentration in Employee Benefits. Throughout the summer, Vincent will be assisting...
Read More
Innovative Welcomes Patrick Scher
Please join us in welcoming Innovative’s new Benefits Consultant, Patrick Scher. Patrick graduated from Penn State University in 2017 with a B.S. in Corporate Innovation and Entrepreneurship. While in school, Patrick was a summer intern with Arthur J. Gallagher & Co. in Radnor, PA. Prior to joining the Innovative team,...
Read More
Innovative Speaks at Leading Age NJ Annual Meeting & Expo
Last Wednesday, the Innovative team had the pleasure exhibiting and presenting at the Leading Age New Jersey Annual Meeting & Expo at Harrah’s Casino in Atlantic City, NJ. Innovative representatives, Dan Foley and Ryan Kastner, presented **Bucking the Trend: _Health Plan Cost Containment Strategies_** to an audience of aging services providers....
Read More
Innovative Wellness Client’s Huge Loss is a Big Win
Congratulations to the Penndel Mental Health Center employees who participated in Innovative Workplace Wellness’ “Three Keys Challenge” coordinated by our Wellness Coordinator, Erica Brown. The “Three Keys Challenge” is a proprietary three-month team weight loss program that encourages participants to focus on three key factors that contribute to long-term weight...
Read More
Compliance Alert! – NJ Gov. Phil Murphy Signs Two New Healthcare Acts into Law
This past week, New Jersey Governor, Phil Murphy, signed two bills into law that will impact New Jersey residents. Employers who offer benefits in New Jersey and surrounding states should be mindful of these changes as they will affect employees who reside and/or receive medical treatment in New Jersey. Out-of-network...
Read More
Horizon BCBSNJ Changes Coverage for Brand Name Oral-Combined Contraceptives
Starting June 15, 2018 , Horizon Blue Cross Blue Shield of New Jersey will be making changes to the way brand name oral-combined contraceptives are covered. Previously covered with a $0 copay, brand name oral-combined contraceptives will now be subject to co-payment or coinsurance that corresponds with the member’s pharmacy...
Read More
Innovative Welcomes Ann Lipiros
This week, Innovative welcomes our newest team member, Ann Lipiros. Ann graduated with a bachelor’s degree in Marketing from St. John’s University in New York. She has experience as a retail Assistant Manager and a Benefits Account Manager. Ann will be supporting our Account team as a Benefit Guardian, serving...
Read More
Innovative Sits Comfortably with Strive
Innovative Benefit Planning has partnered with Strive Physical Therapy to combat the ill effects of a sedentary lifestyle. On Friday, May 18th Jason Melnyk from Strive met with Innovative Benefit Planning employees to educate the team on all of the intricacies of desk ergonomics during their “DeskFit” lecture. The “DeskFit” session...
Read More
IRS Releases 2019 Calendar Year HSA Contribution Limits and HDHP Deductible Minimums and Out-of-Pocket Maximums
The IRS has released the maximum contribution limits for Health Savings Accounts (HSAs) and High Deductible Health Plan (HDHP) minimum deductibles and out-of-pocket maximums for the 2019 Calendar Year. For your convenience, we’ve provided a summary below. You can reference the official document here. Health Savings Account contribution limit for...
Read More
New Jersey Paid Sick Leave Act Signed into Law
New Jersey has now become the tenth state to enact a statewide mandatory paid-sick-leave law. The New Jersey Paid Sick Leave Act was signed into law on May 2nd by Gov. Phil Murphy and will go into effect on Oct. 29, 2018. Once effective, it will require New Jersey employers...
Read More
2018 Health Savings Account Contribution Limits Change Once Again
If you recall, after the passing of the tax reform bill, known formally as the Tax Cuts and Jobs Act, the IRS adjusted the amount for HSA family contributions from $6,900 to $6,850 due to a change in inflation calculations. After public outcry and consideration of the administrative and financial...
Read More
New Jersey Newborn Mandate Changes in 2018
In January 2018, the State of New Jersey updated the existing NJ Newborn Mandate that provides health coverage for all newborns from the moment of birth for the first 31 days to provide coverage from the moment of birth for the first 60 days. The newborn child of a subscriber...
Read More
March Compliance Recap
March was a quiet month in the employee benefits world. The Internal Revenue Service (IRS) released a bulletin that lowered the family contribution limit for health savings account (HSA) contributions. The U.S. Department of Labor (DOL) updated its model Premium Assistance Under Medicaid and the Children’s Health Insurance Program notice...
Read More
PrimeMail by Walgreens Gets a New Name
Effective 3/31/2018 PrimeMail by Walgreens Mail Service will operate under the name “Alliance RX Walgreens Prime“. Prime + Walgreens assures customers that only their name is changing. AllianceRX Walgreens Prime promises to stay consistent with their standards for communications, prescriptions, refills and service. Employers who have health plans with Horizon...
Read More
The Importance of Wellness in the Workplace
Workplace Wellness is an investment which works much like any other investment- You put in time and money in hopes of a more valuable outcome, which in this case is the health of your employees, their families and your bottom line. Engagement, motivation, strategy, and support are the keys to...
Read More
Innovative Welcomes Mima Jovanovic
Please join us in welcoming Innovative’s new Benefit Consultant, Mima Jovanovic. Mima Jovanovic is an accomplished employee benefits consultant with over 20 years of experience cultivating new business opportunities and developing strategic health and welfare programs. He brings a unique perspective to clientele; with significant experience and skills on both...
Read More
IRS RECALCULATES 2018 HSA & EMPLOYER ADOPTION ASSISTANCE PROGRAMS
Yesterday, the Internal Revenue Service (IRS) released a bulletin that includes a change impacting contributions to Health Savings Accounts (HSAs) and Employer Adoption Assistance Programs. The family HSA contribution for 2018 has been reduced from $6,900 to 6,850. This change is effective January 1, 2018. We advise plan participants to...
Read More
Innovative Heads to Capitol Hill
Earlier this week Dan Foley, Ryan Kastner & Yesenia Perez from the Innovative team headed to Washington D.C. for the NAHU 2018 Capitol Conference. During their time in Washington, the trio attended a number of informative sessions that detailed changing legislation that directly impacts the health insurance market and engaged...
Read More
Focusing on FMLA
Human Resource professionals are often asked by their employees about taking a leave of absence. Sometimes, these leaves of absences are protected by the federal government. The Family and Medical Leave Act (FMLA) entitles eligible employees of covered employers to take unpaid, job-protected leave for certain medical and family reasons....
Read More
Innovative Supports Samaritan Healthcare & Hospice
Innovative is proud to support long-time partner, Samaritan Healthcare & Hospice, as a gold sponsor at tomorrow night’s annual Celebration of Life Gala. The event will be held at the Crowne Plaza in Cherry Hill, NJ. Gala proceeds support the gift of hospice, palliative, and grief support services for all Samaritan patients...
Read More
January Compliance Recap
January was a busy month in the employee benefits world. On January 24, 2018, the U.S. Senate confirmed Alex Azar as the new Secretary of the U.S. Department of Health and Human Services (HHS). The U.S. Department of Labor (DOL) proposed regulations regarding association health plans. HHS released the 2018...
Read More
Non-Profit Wager Win Makes the Eagles Victory Even Sweeter
After the Philadelphia Eagles secured their spot in Super Bowl LII, Innovative made a friendly wager with fellow United Benefit Advisors (UBA) partner firm, Employee Benefit Solutions (EBS) out of Massachusetts. The terms were simple- if the Eagles won, EBS would donate $500 to a Philly-area non-profit of Innovative’s choice...
Read More
Preventing Sexual Harassment in the Workplace
As you may have noticed, with an increase in media coverage regarding sexual harassment in the workplace, now is a good time to think about your company’s practices. Does your company have a sexual harassment policy? Are you confident that the sexual harassment policy has been recently updated and that...
Read MorePutting Our Money Where Our Mouth Is!- Superbowl 2018
The Innovative team is getting ready for The Philadelphia Eagles to _ make history _ when they take down the New England Patriots in this Sunday’s Super Bowl. We’ve decided to have a little fun and team up with Employee Benefit Solutions (EBS), a United Benefit Advisors (UBA) partner firm...
Read More
Innovative Welcomes Jay O’Brien
We are excited to announce Innovative’s new Vice President of Financial Operations, Jay O’Brien. Jay will be enhancing our financial account management services and run day-to-day operations. He will also be instrumental in developing our wealth management offering. More about Jay Jay grew up on Long Island and moved to...
Read More
Trump Signs Bill to Delay Cadillac and Health Insurance Taxes
On January 22, 2018, the U.S. Congress voted to pass a bill that would continue to fund the government through February 8, 2018. President Trump signed the bill today, January 23, 2018. In addition to continuing government funding, the bill also includes two legislative victories for employers: delaying the Cadillac...
Read More
Innovative Welcomes Greg Blemlek
Please join us in welcoming Innovative’s new Director of Business Development, Greg Blemlek! Greg has worked in sales & overall growth leadership roles for most of his career. Most recently, Greg had the responsibility of leading a large regional sales and consulting team. During this time, Greg focused on growing...
Read More
December Compliance Recap
December was a relatively busy month in the employee benefits world. The Internal Revenue Service (IRS) delayed the reporting deadlines in 2018 for the 1095-B and 1095-C forms to individuals. President Trump signed the Tax Cuts and Jobs Act. The Centers for Medicare and Medicaid Services (CMS) released guidance on...
Read More
IRS Announces Extension for Furnishing 1095-B & 1095-C Forms to Employees
Recently, the Internal Revenue Service announced an extension for employers to provide 1095-B or 1095-C Forms to their employees. The IRS announced a 30-day extension, extending the due date from January 31, 2018 to March 2, 2018. The IRS has not announced an extension for filings to the IRS. Therefore,...
Read More
Innovative Supports Oaks Integrated Care
This holiday season, the Innovative team has been collecting for Oaks Integrated Care‘s Holiday Giving Drive. Oaks Integrated Care is a non-profit organization that supports adults, children and families throughout New Jersey during vulnerable and turbulent times through a variety of health and social services. The Innovative team came together...
Read More
Innovative Team Decorates Company Tree on Main Street
Last night, a group of Innovative employees made their way down to Moorestown’s Main Street where we decorated Innovative’s company tree. Innovative’s tree is one of a handful of trees lining Main Street this holiday season for the Moorestown Business Association. Our tree features snowmen made by each of our...
Read More
IRS to Send ACA Penalty Letters
The Internal Revenue Service (IRS) has indicated that it plans to begin notifying employers by year end of their potential liability for failing to provide sufficient health coverage that is compliant with the Patient Protection and Affordable Care Act (ACA). The agency will begin notifying Applicable Large Employers (ALEs) of...
Read More
Innovative Partners with Morey’s Piers & Beachfront Water Parks
Innovative is excited to announce our new partnership with Morey’s Piers & Beachfront Water Parks. Morey’s Piers, located in Wildwood, New Jersey is an iconic seaside amusement park comprised of three amusement piers and two beachfront waterparks beloved by beachgoers far and wide. Innovative has been selected as the Benefit...
Read More
Innovative Gets in the Holiday Spirit
This year, the Moorestown Business Association will be lining Moorestown’s Main Street with festive trees sponsored by local businesses. This afternoon, Innovative employees enjoyed a team lunch and decorated personalized ornaments for our company tree. The decorations for our tree reflect our organization’s core values- putting people first, creating & embracing...
Read More
Lunch N’ Burn
As a part of our “Fall Fun & Fitness Challenge” the Innovative team took part in a “Lunch N’ Burn” this afternoon lead by Innovative’s Wellness Coordinator, Erica Brown. After a healthy lunch, Erica lead the team in a “Deskercise” circuit. The team members all received resistance bands and guided...
Read More
Innovative Attends Urban Affairs Coalition Breakfast
On Friday morning, the Innovative team proudly supported our client, Urban Affairs Coalition, at the 48th Anniversary Breakfast at the Pennsylvania Convention Center. Over 800 guests came together to support the mission of the UAC – to unite urban communities to improve the quality of life, build wealth and solve emerging...
Read More
Innovative Accepts Lifetime Achievement Award at National Philanthropy Day Breakfast
A handful of employees from the Innovative team attended the National Philanthropy Day Breakfast at the Mansion on Main Street this morning. The breakfast, coordinated by the Association of Fundraising Professionals of Southern NJ Chapter, celebrated several local honorees who contribute to the success of fundraising in South Jersey. Innovative...
Read More
Innovative Welcomes Shannon Palmucci and Kimberly Fisher
The Innovative team is growing again! We recently welcomed two new employees, Shannon Palmucci and Kimberly Fisher. Shannon attended Rider University where she majored in Accounting. She is joining Innovative as an Account Associate with an extensive background in customer service including 5+ years of experience specializing in benefit administration,...
Read More
Innovative Kicks off Fall Fun & Fitness Challenge with Barre & Balance Class
From November 1st through December 20, the Innovative team is partaking in a “Fun & Fitness” Fall Challenge organized by Innovative’s Wellness Coordinator, Eric Brown. The challenge is comprised of a number of fitness activities with corresponding point values. Employees are encouraged to engage in a variety of healthy activities...
Read More
Fiduciary Rule Update
As you may remember, major components of the Department of Labor (DOL) fiduciary rule have been applicable to retirement advice since June 9, 2017. However, on November 2, 2017, the DOL sent a final rule that would extend the transition period of its fiduciary rule by 18 months to the...
Read More
DOL Overtime Rule Defeated in Court, DOL to Appeal
As you may recall, the Department of Labor put forth overtime regulations that would have taken effect last December, enabling 4.2 million employees to be eligible for time and a half wages for every hour worked over the standard 40 hours per week. However, a number of business groups filed...
Read More
Innovative Supports Steps for Seizures
Members of the Innovative team spent this past Saturday at the Steps for Seizures 5k at Washington Lake Park in Sewell, NJ. The event was hosted by Clayton’s Hope Organization which raises funding for Epilepsy research, awareness and support. The team walked in support of Elisha’s Mission, a cause dedicated...
Read More
Innovative Celebrates Halloween with a Healthy Twist
The Innovative staff enjoyed a fun day at the office this Halloween with visits from a few of the employees’ children and furry friends. The team was treated to a healthy lunch complete with nutritious Halloween-themed desserts prepared by our Wellness Coordinator, Erica Brown and Retirement Plan Specialist, Nicole Offerman....
Read More
Innovative Wins Small Business Award from South Jersey Biz
Innovative is proud to announce that we were recognized in South Jersey Biz Magazine as one of the “Small Business Award” winners! We are excited to be recognized by the local community and named alongside some of the most successful small businesses in the region. Check out our section on...
Read More
Innovative Supports Resources for Human Development
Innovative’s Terriann Procida and Mark Sulpizio were honored to be Jerry Miller’s guest to the Resources for Human Development‘s October 18th annual_Main Line Wine Gala._ Proceeds from the gala support four wonderful initiatives of Resources for Human Development. Terriann and Mark happily purchased a wonderful piece of artwork created by an artist from...
Read More
IRS Releases Maximum Contribution, Deferral and Compensation Limits for HSA, FSA, and 401(k) for 2018
The IRS has released the maximum contribution limits for Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs) for 2018. The IRS also released the maximum deferral and compensation limits for 401(k) accounts. Health Savings Accounts Single Coverage Maximum Contribution Limit: $3,450 ($50 increase from 2017) Family Coverage Maximum Contribution...
Read More
Innovative Supports the 13th Annual Moorestown Progressive Dinner
Innovative Benefit Planning proudly sponsored the Oaks Integrated Care 13th Annual Moorestown Progressive Dinner on Friday, October 13th. Guests gathered at a number of volunteer host homes throughout Moorestown and enjoyed meals prepared by volunteer chefs from some of the area’s most popular restaurants and caterers. Proceeds from the event...
Read More
President Trump Ends ACA Cost Sharing Reductions
On the evening of October 12, 2017, President Trump announced that cost sharing reductions for low income Americans in relation to the Patient Protection and Affordable Care Act (ACA) would be stopped. The Department of Health and Human Services (HHS) has confirmed that payments will be stopped immediately. It is...
Read More
Innovative Welcomes Luke Howard
Please join us in welcoming Innovative’s new Data Analyst, Luke Howard. Luke has a B.S. in Chemical Engineering and during his schooling he was heavily focused on research for sustainability in conjunction with the EPA. He worked primarily with major manufacturers such as DuPont and Nestle in wastewater purification. Luke...
Read More
Compliance Alert!
Two tri-agency (Internal Revenue Service, Employee Benefits Security Administration, and Centers for Medicare and Medicaid Services) Interim Final Rules were released and became effective on October 6, 2017, and will be published on October 31, 2017, allowing a greater number of employers to opt out of providing contraception to employees...
Read More
Innovative to be Honored for Lifetime Achievement for Philanthropy
Innovative is honored to announce that the Association of Fundraising Professionals of Southern New Jersey will be honoring Innovative Founders, Terriann Procida and Mark Sulpizio, with the Lifetime Achievement Award at the 9th Annual National Philanthropy Day Celebration. Terriann and Mark will be honored for their contributions to the success...
Read More
Ryan Kastner Moderates NPDC HR Breakfast Panel
This morning at Adelphia Restaurant & Lounge in Deptford, NJ the Nonprofit Development Center of Southern New Jersey held a breakfast panel discussion for Nonprofit Human Resource professionals. The panel discussion focused on various talent management issues in the nonprofit community. Innovative’s Employee Benefits Consultant, Ryan Kastner, had the pleasure...
Read More
Ryan Kastner Speaks at Pennsylvania State SHRM Conference
Earlier this morning, Innovative’s Employee Benefits Consultant, Ryan Kastner, had the pleasure of presenting at the Pennsylvania State SHRMconference in State College, PA. Ryan’s presentation, “Healthcare Trends in the Trumpcare Era” detailed the most recent national and regional employer health plan trends from the United Benefit Advisor’s Annual Health Plan...
Read MoreInnovative Employer Identity Monitoring and Restoration Services
Recently, Innovative had the pleasure of seeing Frank Abagnale speak at the UBA Conference in Chicago. You may recognize Frank’s name from the movie “Catch Me If You Can” where he was played by Leonardo DiCaprio. Frank became (in)famous for writing fake checks (among other things) as a teenager. Later...
Read More
Post-Equifax Cyber Breach: Retirement Plan Sponsor Considerations
Plan sponsors have a fiduciary obligation to safeguard and preserve the assets of their employee benefit plans. As the number of cyber hacks continues to increase, plan fiduciaries must take certain steps to protect plan assets. Measures include evaluating security measures currently implemented by your organization, understanding the plan’s service...
Read More
Post-Equifax Cyber Breach: Employer and Human Resource Considerations
Under EEOC regulations, employers can utilize credit checks when hiring employees, provided that the information is relevant to the position. For example, an individual who will be responsible for providing sound investment advice to clients, must prove to the company that their own credit is satisfactory. However, many vendors sell...
Read More
DOL Fiduciary Rule Delay Approved by Office of Management and Budget
As you may be aware, the Department of Labor requested to push back the final implementation date of the fiduciary rule, originally scheduled for January, to July 2019. The 18-month delay was approved by the Office of Management and Budget (OMB) of the White House this week. While the delay...
Read MoreRegarding the New York Paid Family Leave Law
NEW YORK PAID FAMILY LEAVE LAW Eligible employees will be able to take NYPFL to take care of a seriously ill family member, to bond with a newborn, adopted or foster child, or for military exigency, as defined by the federal FMLA rules. The New York Disability Benefits Law (NYDBL)...
Read More
July Compliance Recap
July was a relatively quiet month in the employee benefits world, despite the U.S. Senate’s release of two bills in its attempt to repeal the Patient Protection and Affordable Care Act (ACA). First, the U.S. Senate revised its Better Care Reconciliation Act and declined to vote on its revision. Then...
Read More
ACA/BCRA Update
As you know, a few weeks ago Senate Republicans drafted a bill, the Better Care Reconciliation Act (“BCRA”), in an effort to repeal and replace the Patient Protection and Affordable Care Act (“ACA”). If you remember, Republicans currently hold a 52-member majority in the Senate, therefore Senate Republicans are left...
Read More
June Compliance Recap
June was an active month in the employee benefits world. The U.S. Senate released a draft of the Better Care Reconciliation Act of 2017 which would substitute the U.S. House Resolution 1628 that aimed to repeal and replace the Patient Protection and Affordable Care Act (ACA). The U.S. Supreme Court...
Read More
PCORI FILING DUE TO IRS BY JULY 31
It’s that time of year again for PCORI fees to be paid. As you may already know, the Affordable Care Act established the Patient-Centered Outcomes Research Institute (PCORI). The purpose of PCORI is to promote research efforts that will help Americans make better informed health decisions. To fund this effort,...
Read More
DOL Releases Additional Guidance Regarding the Fiduciary Rule
As part of our commitment to ensuring that our clients are kept up-to-date on the changes to applicable laws, the Department of Labor (DOL) has released additional guidance regarding the Fiduciary Rule. In our recent blog post, we discussed the applicability date of the Fiduciary Rule being delayed from April...
Read More
Innovative & Ryan Kastner Honored at Annual United Way Awards Celebration
This Thursday, May 18th, the Innovative team attended the Annual United Way of Burlington/Camden Counties Awards Celebration at the Ramblewood Country Club in Mount Laurel, NJ. Innovative was honored to receive the “Culture of Caring” Award for organizations with outstanding employee participation rates. Innovative’s Employee Benefits Consultant, Ryan Kastner, was...
Read MoreThe CHOICE Act and its Impact on the Fiduciary Rule & Dodd-Frank
Late last week, the House Financial Services Committee approved the CHOICE Act for consideration by the full House of Representatives. The CHOICE Act is likely the first step towards Congressional repeal of the Department of Labor’s fiduciary rule. In addition to undoing or potentially replacing the Dodd-Frank Wall Street reform...
Read MoreFloat Your Way to Better Health
Every day, 24 hours a day, 7 days a week, our senses are being stimulated by light, sound, and other sensations. Our muscles and bones are working hard against gravity to support us with each movement that we make. If we are not careful to take care of our bodies,...
Read More
DOL Delays Applicability Date of the Fiduciary Rule
As you are likely aware, the Department of Labor proposed a delay to the Fiduciary Rule on March 1, 2017 in response to President Trump’s Executive Order. On April 4, 2017, the DOL made their final rule public and have delayed the applicability date to June 9, 2017. It will...
Read More
March Compliance Recap
In March, the employee benefits world watched as the House Speaker unveiled a proposal to replace parts of the Patient Protection and Affordable Care Act (ACA) with the American Health Care Act (AHCA). The AHCA bill was withdrawn from consideration by the full House on March 24 because it appeared...
Read More
Innovative Spotlight- Yesenia Perez, JD, LLM
Innovative Spotlight Yesenia Perez, JD, LLM is pioneering the role of Compliance Counsel at Innovative Benefit Planning. Facing constant challenges of the ever-changing insurance industry and the impact the Affordable Care Act has had on employers nationwide, we knew we needed more compliance support for our clients. Yesenia has been...
Read More
February Compliance Recap
February had relatively little activity in the employee benefits world because a new Secretary of the Department of Health and Humans (HHS) was recently confirmed and HHS started its rulemaking under the new administration. On February 10, 2017, the U.S. Senate confirmed Rep. Tom Price as the new Secretary of...
Read More
Innovative Welcomes Jennifer Berwick
Innovative is happy to announce the newest addition to our team, Jennifer Berwick. Jennifer comes to us with a diverse background in office administration and accounting. She will be working closely with Innovative’s CEO, Teriann Procida, where she will look to leverage her organizational talents to help Innovative’s office run...
Read More
Impact of Opt-Out Incentives on ACA Affordability Calculations
Quick Overview of Affordability Employers may find themselves subject to a penalty if an employee goes to the Marketplace/Exchange and obtains a premium credit, because the employer plan was not affordable or does not provide minimum value. An employee is not eligible for a premium tax credit for...
Read MoreProposed Regulations Allow for Permitted Uses of Plan Forfeitures in a 401(k) Plan
On January 18, 2017 the IRS issued proposed regulations that allowed for permitted uses of plan forfeitures in a 401(k) plan. Under these proposed rules, “Qualified Nonelective Contributions, or QNCEs and “Qualified Matching Contributions” or, QMACs would be amended to allow plan sponsors to use amounts held in the plan’s...
Read MoreThe fate of the Fiduciary Rule
As you may know, on Friday, February 3, 2017, President Trump signed a memorandum directing the Department of Labor Secretary to undertake a new “economic and legal analysis” to evaluate the Fiduciary Rule. To the extent that the new analysis reveals any issues, the Labor Secretary is directed to publish...
Read More
Innovative Welcomes Shannon Thomson
The Innovative team continues to grow with our most recent addition to the team, Shannon Thomson. Shannon was most recently the Executive Administrative Assistant for the Sports & Entertainment department at Aramark. She is currently working on completing her degree in Business Administration at the University of Phoenix. Shannon joins...
Read MoreRyan Kastner Included in South Jersey Magazine’s 2016 Men of the Year
Please join us in congratulating Innovative’s Employee Benefits Consultant, Ryan Kastner, on being included in South Jersey Magazine‘s 2016 Men of the Year. Ryan was one of fifteen men in the South Jersey area recognized for their philanthropic efforts and contributions to their local communities. To read more, check out...
Read MoreNovember 2016- Compliance Recap
November was quite an active month for compliance related updates in the law with regard to employee benefits and human resources. The IRS delayed 6055 and 6056 reporting for 2017, the Overtime Rule was delayed, the government released annual benefit plan amounts for 2017, and the IRS released advanced copies...
Read MoreCompliance Alert! – DOL Appeals FLSA Overtime Rule Injunction
As we expected, last evening, the Department of Labor filed a notice of appeal in the Fifth U.S. Circuit Court of Appeals in New Orleans. The Department of Labor’s appeal indicates plans to challenge the injunction that put the changes to the federal overtime rule on hold by a Texas...
Read MorePhishing Email Alert
The Department of Health and Human Services has issued an alert regarding phishing attempts by a company or individual utilizing the HHS Departmental letterhead under the signature of OCR’s Director. The email appears to be an official government communication and targets employees of HIPAA covered entities and their business associates....
Read MoreFLSA Overtime Rule Blocked by Federal Judge
On Tuesday, November 22, 2016, a Texas federal judge blocked the Fair Labor Standards Act Overtime Rule by issuing a nationwide preliminary injunction. The regulation was scheduled to take effect on Dec. 1 and would have raised the salary limit for which workers could be exempt for overtime pay from...
Read MoreIRS Extends 1095 Deadline
The Internal Revenue Service has just announced an extension on the 2016 Form 1095-C , Employer Provided Health Insurance Offer and Coverage. Previously, the 1095-C was due to full time employees on January 31, 2017. Although the IRS had previously indicated not to expect an extension, an extension was granted...
Read More
The Trump Administration & Healthcare Reform
On January 20, 2017, Donald J. Trump will be sworn in as the next President of our nation. Next year, Republicans will have the majority in the House of Representatives (238 Republicans, 191 Democrats) and the majority in the Senate (51 Republicans, 47 Democrats). On November 14, 2016, House Republicans...
Read More
October 2016 Compliance Recap
October was a busy month for administrative rule-making in the employee benefits world. The Internal Revenue Service (IRS) released final instructions for Forms 1094-C and 1095-C, guidance on the taxability of health care sharing ministry employer contributions, and health care information reporting tips. The Department of Health and Human Services...
Read More
Innovative Welcomes New Worksite Wellness Consultant
We are happy to announce the newest addition to our team, Erica Brown. Erica will be taking over the role of Worksite Wellness Consultant and will be responsible for overseeing the development and implementation of worksite wellness programs for Innovative’s clients. Erica Brown is a seasoned Nutritionist and Wellness Coach...
Read More
October 27th- A Night of Celebration
The Innovative team had lots to celebrate last Thursday night! Spread throughout the Philadelphia/South Jersey area, the Innovative team celebrated our Philadelphia 100 win at the Filmore in Philadelphia, our SNJBP Reader’s Choice awardin Insurance and Risk Management at Lucien’s Manor in Berlin, NJ and our Employee Benefits Consultant, Ryan Kastner’s...
Read More
The Shift to Self-Funding
Year over year, more employers are making the switch from fully-insured health plans to self-funded arrangements. As of 2015, 63% of all covered employees are on completely or partially-funded employer health plans. Innovative Employee Benefits Consultant, Ryan Kastner, was quoted in MedCity News discussing the intricacies of self-funding. To read the...
Read More
Compliance Recap- September 2016
September was not a very active month for administrative rulemaking in the employee benefits world. The Internal Revenue Service (IRS), Department of Labor (DOL), and Pension Benefit Guaranty Corporation (PBGC) extended the public comment period for the proposed Form 5500 annual return/report revision. The IRS issued rules defining terms relating...
Read More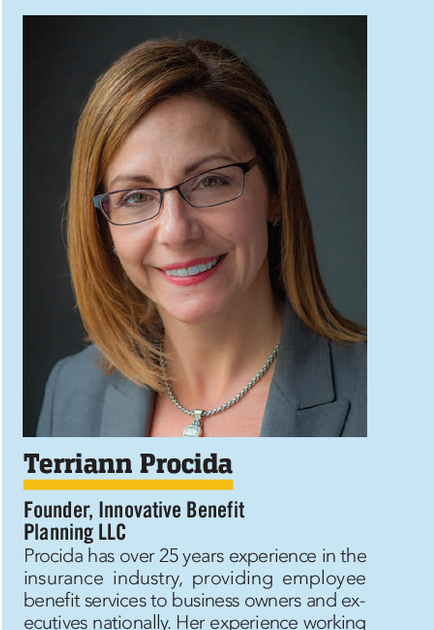
Innovative’s CEO Named “Outstanding Entrepreneur” by South Jersey Biz
South Jersey Biz Magazine named Innovative’s CEO, Terriann Procida, as one of their “Outstanding Entrepreneurs” in their September 2016 publication. We are so proud of Terriann, who was named alongside a select group of successful entrepreneurs in the South Jersey area, all of whom took great risks in business and are now...
Read More
Innovative Takes on The Spartan Race
This past Saturday, September 24th, Innovative CEO, Terriann Procida, joined by Employee Benefits Consultants Ryan Kastner and Sean Healy and her sons, Elias and Will, took on the Reebok Spartan Race at Citizens Bank Park in Philadelphia, PA. The course consisted of a number of grueling obstacles including rope climbing, wall climbing, monkey...
Read More
Innovative Attends United Benefit Advisor’s Fall Conference in Chicago
The Innovative team headed to Chicago this past weekend for the United Benefit Advisor’s Fall Conference September 18th-20th. “UBA is the nation’s leading organization of independent benefit advisors who are bound by a code of conduct to actively cultivate, validate and share wisdom with busy benefit decision makers nationwide who want...
Read More
Innovative Honored to Receive 2016 Readers’ Choice Award
For the second year in a row Innovative Benefit Planning, L.L.C. is proud to announce that we were voted a Leader in Insurance and Risk Management in SNJBP‘s 2016 Readers’ Choice Awards. We are thrilled to be acknowledged by the SNJBP readers, who hail from Burlington, Camden and Gloucester Counties. These communities are home...
Read More
How Corporate Wellness Programs Benefit You and Your Organization
Has your organization adopted a structured wellness program? Many employers are resistant to kickoff corporate wellness programs due to lack of knowledge and fear of high start up costs and increasing the workload on their busy Human Resources department. Read more in our Wellness Program Whitepaper about how you can...
Read More
August Compliance Recap
August remained relatively quiet in the employee benefits world, with only new draft versions of the instructions for Forms 1095-C, 1095-C, 1094-B and 1095-B. The new draft versions of the specific forms were released in July. The IRS also released the annual contribution limits for health savings accounts (HSAs) and...
Read More
August Compliance Recap
August was quiet month in the employee benefits world. The Internal Revenue Service (IRS) released its 2018 affordability rate, four information letters regarding the Patient Protection and Affordable Care Act (ACA), and its draft Forms 1094 and 1095. The U.S. Department of Labor (DOL) increased the McNamara-O’Hara Service Contract Act...
Read More
Innovative Included in 2016 Philadelphia 100!
We are proud to announce that Innovative has been included in the 2016 “Philadelphia 100” list! The Philadelphia 100 is an annual project run by the Wharton Small Business Development Center and The Entrepreneur’s Forum of Greater Philadelphia. Innovative is honored to be named in this merit-based program alongside the fastest...
Read More
The Top 5 Things to Look for in an ACA Reporting Consultant
Innovative Benefit Planning’s consultants are widely considered the Affordable Care Act experts in the Greater Philadelphia and New Jersey areas. While many employers struggled with the ACA reporting for 2015 with little support, Innovative clients slept easy with employee communications, in-depth consultations, pre-form data audits, and error resolution support. Innovative...
Read More
HRAs, HSAs, and Health FSAs – What’s the Difference?
Health reimbursement arrangements (HRAs), health savings accounts (HSAs) and health care flexible spending accounts (HFSAs) are generally referred to as account-based plans. That is because each participant has their own account, at least for bookkeeping purposes. Under the tax rules, amounts may be contributed to these accounts (with certain restrictions)...
Read More
Innovative Named “Best of the Biz” 2016
Innovative is proud to announce that we were named “Best of the Biz 2016” in South Jersey Biz‘s August issue! Annually, South Jersey Biz complies a “Best of the Biz” list through readers’ and editors’ selections. Innovative is honored to be recognized by South Jersey Biz readers in the category of Benefit Consultant....
Read More
Employment Eligibility: How to Handle Questions about Worker Identity
Reports submitted to the U.S. government that include both names and Social Security numbers (SSNs), such as 1095 and W-2 forms, are filtered through U.S. Immigration and Customs Enforcement (ICE), a division of the Department of Homeland Security (DHS). In some cases, employers will receive a No-Match Letter or an...
Read More
Compliance Recap- July 2016
During the month of July numerous new regulations were issued or proposed by federal agencies, and existing forms and processes were updated. In particular, penalties for various ERISA violations were increased, a major overhaul to Form 5500 filings was proposed, and draft 1095-C and 1094-C forms were released. Proposed regulations...
Read More
Salary Considerations under the New DOL Standards
On December 1, 2016, the Department of Labor (DOL) will implement changes raising the minimum compensation for exempt employees to $47,476 annually. While salary is just half of a two-part equation that includes a duties test of essential job functions, scrutiny is under way to analyze compensation and find solutions...
Read More
June 2016 Compliance Recap
June was another quiet month for federal agencies in relation to employee benefits. A tri-agency proposed rule regarding expatriate health plans, excepted benefits, and essential health benefits was released. UBA Updates UBA’s Human Resources department released a checklist and advisor on new OSHA requirements: OSHA Reporting Changes: Employer Checklist OSHA’s...
Read More
Innovative’s CEO Honored at 2016 Brava Awards
Last night, the Innovative team gathered at the Crystal Tea Room in Philadelphia to celebrate Innovative’s CEO, Terriann Procida, as she was presented with SmartCEO‘s 2016 Philadelphia Brava Award. The Brava Award is bestowed upon female business leaders in the greater Philadelphia area who possess incredible leadership qualities both within...
Read More
Interim Final Rule Updating the Penalties for Certain ERISA Violations
In the beginning of July, the Department of Labor (DOL) issued an interim final rule, effective August 1, 2016, adjusting the amounts of civil penalties as required by the Federal Civil Penalties Inflation Adjustment Act Improvements Act of 2015. In order to improve the effectiveness of civil monetary penalties, maintain their deterrent...
Read More
Proposed Rule Offers Guidance on Expatriate Health Plans, Excepted Benefits and Essential Health Benefits
In a tri-agency proposed rule, the Department of Labor (DOL), Department of Health and Human Services (HHS), and Department of Treasury (Treasury) have published guidance discussing expatriate health plans (expat plans), excepted benefits, and essential health benefits (EHBs). Expatriate Health Plans The proposed rule would allow expatriate health plans, employers...
Read More
1095/1094 Reporting Accepted…with Errors?
Ryan Kastner – Employee Benefits Consultant Mid and large size employers have begun to breathe a sigh of relief knowing the first year of 1095/1094 Reporting is almost behind us. Unfortunately, 70% of employers are unable to fully relax as many are receiving notices of “filing discrepancies” within their 1095...
Read More
Innovative Presents at the BPAS Annual Conference
The Innovative team spent June 6, 7 and 8, 2016 at the Benefit Plans Administrative Services (BPAS) Annual Partner Conference in Philadelphia. The annual conference draws financial intermediary partners from across the country for three days of panels and breakout sessions covering a variety of topics including: technical and legislative updates, fiduciary...
Read More
Terriann Participates in SmartCEO’s “Think Tank” Discussion
On June 7th, Innovative President, Terriann Procida, joined a group of fellow Philadelphia-area Brava winners to participate in SmartCEO‘s “Think Tank” discussion hosted by Comcast Business on Corporate Social Responsibility and Philanthropy. Panelists spoke on the various ways their businesses engage with their local communities, how their organization’s productivity and employee...
Read More
OSHA Issues a Final Rule on Electronic Tracking of Workplace Injuries & Illnesses
Is your organization tracking workplace illnesses and injuries in accordance with new laws? Beginning in 2017, certain employers with as few as 20 employees at a single site will be required to electronically file information about employee injuries and accidents that occurred in the prior year. This means that, for many...
Read More
Ryan Kastner Selected as “20 Under 40!”
More great news! We are proud to announce that Innovative’s Employee Benefits Consultant, Ryan Kastner, was named one of South Jersey Biz‘s “ 20 Under 40! ” Annually, South Jersey Biz honors the accomplishments of young professionals under the age of 40 in the South Jersey area through the “20 Under...
Read More
Nondiscrimination Regulations Relating to Sex, Gender, Age, and More Finalized
On May 13, 2016, the Department of Health and Human Services (HHS) issued a final rule implementing Section 1557 of the Patient Protection and Affordable Care Act (ACA), which will take effect on July 18, 2016. If entities need to make changes to health insurance or group health plan benefit...
Read More
What’s Next in ACA Reporting
Now that the first set of reporting forms have been completed, many employers are wondering what the next steps are. Employers that did not fulfill all of their obligations under the employer shared responsibility provision (play or pay) might owe a penalty to the IRS. A penalty will be owed in...
Read More
Congratulations Terriann!
We are proud to announce that Innovative President & Founder, Terriann Procida was selected to receive Smart CEO‘s 2016 Philadelphia Brava Award! The Brava Award celebrates top female CEO’s along the east coast in Baltimore, Boston, Charlotte, Long Island, New Jersey, New York, Philadelphia and Washington. Winners are recognized for their accomplishments...
Read More
Compliance Recap- April 2016
Catch up on compliance developments you may have missed last month with UBA’s April 2016 Compliance Recap. As much of the country anxiously awaits the Department of Labor’s (DOL) long-promised final rule relating to overtime exemption regulations, the employee benefits space has been relatively quiet. March 31 was the first...
Read More
DOL Issues Another FAQ on ACA Implementation
The U.S. Department of Labor (DOL) has issued its 31st FAQ on the implementation of the Patient Protection and Affordable Care Act (ACA), dedicated to coverage of preventive services, rescissions of coverage, out-of-network emergency services, clinical trial coverage, cost-sharing limitations, the Mental Health Parity Act, and the Women’s Health and...
Read More
IRS Reporting: Now What?
Applicable large employers and self-funded employers of all sizes have now completed the first round of required IRS reporting under the Patient Protection and Affordable Care Act (ACA). The ACA requires individuals to have health insurance, while applicable large employers (ALEs) are required to offer health benefits to their full-time...
Read More
Seven Common Mistakes That Could Trigger a DOL Audit
Here are some great tips on how to avoid a DOL audit from the UBA Blog: Not many things incite more fear than receiving a notice that you’re about to have an audit, especially from the Department of Labor (DOL). The DOL is a cabinet-level department of the U.S. federal...
Read More
Innovative Presents “Healthy Eating on a Budget” Seminar
Last Thursday, Innovative’s Wellness Coach, Lori Drouin, and Employee Benefits Consultant, Ryan Kastner, headed to the Occupational Training Center of Burlington County to present the educational wellness program “Health Eating on a Budget” to the Occupational Training Center staff. Lori walked OTC employees through a variety of ways to make healthy food choices, make...
Read More
DOL Announces New Fiduciary Rule
On April 16th, the Department of Labor provided the long awaited revision to the fiduciary definition in the Fiduciary Rule. The new rule has been debated for many months and clarifies what is considered fiduciary advice. Under ERISA, a fiduciary is defined as someone who exercises discretion as to the...
Read More
Compliance Recap – March 2016
The government was busy during the month of March, issuing the massive Benefit Payment and Parameters rule in addition to numerous other updates. The IRS has added filing errors relating to Form 5500 to its project list, and multiple federal agencies confirmed that the just-announced templates relating to the...
Read More
Innovative’s Ryan Kastner Named One of SNJBP’s “40 Under 40!”
Please join us in congratulating Innovative’s Employee Benefits Consultant, Ryan Kastner, on being named “40 Under 40” bySNJ Business People! Last night, Ryan was among 40 local business people under the age of 40 honored for their professional and philanthropic achievements at The Mansion in Voorhees. Southern New Jersey Business People’s ’40...
Read More
IRS Reporting Tip #2 – Form 1095-C, Line 14, Code 1A versus 1E, and When To Use 1I
Under the Patient Protection and Affordable Care Act (ACA), individuals are required to have health insurance, while applicable large employers (ALEs) are required to offer health benefits to their full-time employees. In order for the Internal Revenue Service (IRS) to verify that (1) individuals have the required minimum essential coverage,...
Read More
IRS Reporting Tip #1 – Form 1094-C, Line 22
Under the Patient Protection and Affordable Care Act (ACA), individuals are required to have health insurance while applicable large employers (ALEs) are required to offer health benefits to their full-time employees. In order for the Internal Revenue Service (IRS) to verify that (1) individuals have the required minimum essential coverage,...
Read MoreBenefit and Payment Parameters Rule and HIP FAQ
The 2017 Benefit and Payment Parameters (BPP) rule, an annual rule that sets policies relating to the Patient Protection and Affordable Care Act (ACA), has been released by the Centers for Medicare and Medicaid Services (CMS). The 2017 rule contains numerous updates, including the annual open enrollment periods for the...
Read More
Compliance Recap – February 2016
Despite having an extra day, February 2016 remained relatively quiet in regard to compliance and employee benefit plans. The Department of Labor (DOL) issued the awaited proposed revisions to the Summary of Benefits and Coverage (SBC) template and its instructions. The 2016 poverty guidelines (also referred to as the FPL)...
Read More
Proposed Summary of Benefits and Coverage Template and Updates
A Summary of Benefits and Coverage (SBC) is four-page (double-sided) communication required by the federal government. It must contain specific information, in a specific order and with a minimum size type, about a group health benefit’s coverage and limitations. In February 2016, the Department of Labor (DOL) issued proposed revisions...
Read MoreInnovative Attends 2016 NAHU Capitol Conference
This past week, Innovative representatives Dan Foley and Ryan Kastner headed to Washington D.C. for the National Association of Health Underwriters Capitol Conference. Below are live-tweets from the conference. #NAHUCapCon2016 Met w/ NAHU CEO Janet Trautwein 4 an exclusive UpdateFromTheHill 4 UBA partners. These will be a large part of our...
Read More
Innovative Welcomes Stacey Zielke!
Innovative is happy to announce the newest addition to our team, Stacey Zielke! Stacey, formerly a Benefit Specialist for Benefit Concepts, brings 15 years experience in the Human Resources Field. Stacey graduated from Rider University with a degree in Psychology and earned her PHR Certification in 2006. Stacey recently joined...
Read More
Compliance Recap- January 2016
January was a very quiet month for compliance, on the heels of the multitude of delays that came at the end of December 2015. The IRS updated its FAQs related to 6055 and 6056 reporting under the Affordable Care Act (ACA). UBA Guides and Compliance Documents UBA updated the popular...
Read More
IRS Updates FAQs Related to 6055/6056 Reporting
The long-standing IRS FAQs related to reporting under sections 6055 and 6056 on requirements provided by the Patient Protection and Affordable Care Act (ACA) have been updated in January 2016 to reflect new information. Final instructions for both the 1094-B and 1095-B and the 1094-C and 1095-C were released in...
Read More
Compliance Recap – December 2015
2015 went out with a bang, as federal agencies and the White House issued a number of major delays relating to employee benefits. Most significantly, IRS reporting for the Patient Protection and Affordable Care Act’s play or pay requirement has been delayed, for both forms being sent to employees and...
Read More
IRS Final Rule on Minimum Value
In December 2015, the Internal Revenue Service (IRS) issued a final rule that clarifies various topics relating to the Patient Protection and Affordable Care Act (ACA) and premium tax credit eligibility provisions. The rule finalizes regulations that were proposed years earlier. Child Income The final rule clarified language relating to...
Read More
IRS Provides Major Delay in 6055 and 6056 Reporting
Under the Patient Protection and Affordable Care Act (ACA), individuals are required to have health insurance, while applicable large employers (ALEs) are required to offer health benefits to their full-time employees. In order for the Internal Revenue Service (IRS) to verify that (1) individuals have the required minimum essential coverage,...
Read More
COBRA and the Affordable Care Act
The Consolidated Omnibus Budget Reconciliation Act COBRA requires employers to offer covered employees who lose their health benefits due to a qualifying event to continue group health benefits for a limited time at the employee’s own cost. COBRA provisions are found in the Employee Retirement Income Security Act (ERISA), the...
Read More
Omnibus Bill Signed Into Law; Delays Cadillac Tax
President Obama has signed the omnibus legislation that includes the Consolidated Appropriations Act for 2016 and a tax extenders package. The agreement will keep the federal government running through September 2016. Within the legislation is language that significantly impacts provisions of the Patient Protection and Affordable Care Act (ACA), largely...
Read More
IRS Notice 2015-87: HRAs, Affordability, and More
On December 16, 2015, the Internal Revenue Service (IRS) and other federal agencies released IRS Notice 2015-87, which is a “potpourri” update that covers many different topics relating to the Patient Protection and Affordable Care Act (ACA), including some relating to market reforms. The Notice generally covers health reimbursement arrangements...
Read More
Innovative’s 2015 Gift Exchange
Innovative got into the holiday spirit on Friday with our annual holiday white elephant gift exchange. The team had a great time opening (and stealing) gifts over drinks and delicious food catered by Moorestown’s Maurizio’s Bistro. Here are some photos from the event: [] [] [] [] [] [] [] []...
Read More
Innovative Receives SNJBP Readers’ Choice Award!
Innovative Benefit Planning, L.L.C. is proud to announce that we were voted a Leader in Insurance and Risk Management in SNJBP‘s 2015 Readers’ Choice Awards. Innovative is honored to be recognized by the readers of SNJBP who hail from Burlington, Camden and Gloucester Counties. These communities are home to many of our clients and...
Read More
Proposed Benefit Payment and Parameters Rule Released
Federal agencies have released the proposed rule for the 2017 Benefit Payment and Parameters. Among other items, it provides updates and annual provisions relating to: Risk adjustments, reinsurance, and risk corridors programs Cost-sharing parameters and cost-sharing reductions User fees for Federally-Facilitated Exchanges (FFEs) The standards for open enrollment for the...
Read More
Agencies Issue Final Rule on Grandfathered Health Plans and Other Initiatives
On November 13, 2015, federal agencies issued a final rule that essentially combined a variety of interim final rules and non-regulatory guidance on a variety of Patient Protection and Affordable Care Act (ACA) initiatives such as grandfathered health plans, preexisting condition exclusions, internal and external appeals, rescissions of coverage, lifetime...
Read MoreEEOC Issues Proposed Rule Relating to Genetic Information and Wellness Programs
On October 30, 2015, the Equal Employment Opportunity Commission (EEOC) issued a Proposed rule to amend the regulations implementing Title II of the Genetic Information Nondiscrimination Act (GINA) as they relate to employer wellness programs that are part of group health plans. The Proposed rule would allow employers to offer...
Read MoreThere’s Still Time to Get Help With ACA Reporting For 2015!
As ACA reporting deadlines for the 2015 tax year quickly approach, many organizations have found that the task of 1094/1095 reporting is too arduous to take on internally. At this point in the year, many payroll providers and independent companies have implemented strict registration deadlines for early November. If you are...
Read MoreCMS Provides Clarity on PACE Act Implications for States
The Providing Affordable Coverage for Employees (PACE) Act amended the Patient Protection and Affordable Care Act (ACA) and redefined small employers as those with 50 or fewer employees; it also gives states the option to expand the definition to include employers with up to 100 employees (or, practically speaking, those...
Read MoreMark Sulpizio Named New Board Member of YMCA of Burlington and Camden Counties
Please join us in congratulating Innovative’s Mark Sulpizio on his admission to the Board of Governors of the YMCA of Burlington and Camden Counties! Mark joins a prestigious group of community leaders who volunteer their time and expertise to bring positive change to the region. The YMCA of Burlington and...
Read MoreACA’s Auto-Enrollment Requirement Repealed
The Patient Protection and Affordable Care Act (ACA) initially required employers with more than 200 full-time employees and that offer employees one or more health benefit plans must automatically enroll (and re-enroll existing) full-time employees into one of the health plans (subject to any waiting period authorized by law), in...
Read MoreHalloween at Innovative
Last Friday, the Innovative team got into the Halloween spirit by dressing up and celebrating with friends and family at the 2015 Innovative Halloween party. Guests enjoyed delicious food prepared by Georgetti’s Catering and employees brought Halloween-themed treats for dessert. A big thank you to Mark, Terriann and our Wellness team...
Read MoreDOL Issues FAQ on Mental Health Parity and ACA Market Reform Provisions
In October 2015, the Department of Labor (DOL) provided an informational FAQ relating to the Mental Health Parity and Addiction Equity Act (MHPAEA) and Patient Protection and Affordable Care Act (ACA) market reform provisions. Non-grandfathered group health plans and individual or group market health insurance must cover a variety of...
Read MoreIRS Proposed Regulations Recognize Same Sex Marriage
In June 2015, the Supreme Court ruled in Obergefell v Hodges that the 14th Amendment requires a state to license a marriage between two people of the same sex, and to recognize a marriage between two people of the same sex when their marriage was lawfully licensed and performed out...
Read MoreInnovative Founders Host Moorestown Progressive Dinner
Innovative Benefit Planning was proud to support Oaks Integrated by sponsoring, attending and hosting the 2015 Moorestown Progressive Dinner on October 16th. Innovative Principals, Mark Sulpizio and Terriann Procida, hosted a group of professionals from the Moorestown community for a special dinner prepared by Chef Todd-Jay Annese from Brio Tuscan Grill....
Read MoreInnovative Welcomes Sean Healy!
Innovative is excited to announce the addition of our newest team member, Sean Healy! Sean, formerly a technology sales rep for ADP, brings his 5 years of expertise with HR and benefit administrative technology to Innovative. Sean graduated from Kutztown University with a degree in accounting and later expanded into...
Read MoreUPDATE- “Small Employer” Redefined
On Wednesday evening, President Obama signed into law H.R. 1624, more commonly known as The PACE Act. This new legislation amends the Affordable Care Act and allows individual states to determine how they define small-group markets. Now, it will be up to state legislators to govern whether they will...
Read MoreWe’re growing! Innovative Welcomes Mary Gannon
Innovative is happy to announce the addition of our newest team member, Mary Gannon. Mary is a licensed health insurance professional with over 19 years of experience in the health care industry. Mary worked at IBC and AmeriHealth for many years as an associate representative as well as an account...
Read MorePACE Act Passes House, Senate
The U.S. Senate, following the House of Representatives, has passed House Resolution 1624, the “Protecting Affordable Coverage for Employees Act” or “PACE Act” which will be sent to President Obama’s desk for signature. It is anticipated the President will sign the Act into law. The PACE Act would amend the...
Read MoreIRS Notice on Minimum Essential Coverage Reporting
Minimum essential coverage or “MEC” is the type of coverage that an individual must have under the Patient Protection and Affordable Care Act (ACA). Employers that are subject to the ACA’s shared responsibility provisions (often called play or pay) must offer MEC coverage that is affordable and provides minimum value....
Read MoreInnovative Benefit Planning goes to UBA Chicago
September 12th-September 15th Innovative Benefit Planning team members Terriann Procida, Mark Sulpizio, Scott Agostini, Elizabeth Hann, Caitlin Boland, Ryan Kastner and Dan Foley headed to Chicago, Illinois for the United Benefit Advisors Semiannual Conference. The conference provided many informative “Boot Camp” session on compliance, surveys, marketing and Employee Navigator Training that will help...
Read MorePerfect Attendance! – How to Handle Leaves of Absence under the ACA
The Patient Protection and Affordable Care Act (ACA) requires applicable large employers (ALEs) to offer full-time employees health coverage, or pay one of two employer shared responsibility penalties. An ALE is an employer with 50 or more full-time or full-time equivalent employees (for 2015, this threshold is 100). A full-time...
Read MoreInnovative Welcomes Lori Drouin!
Lori is a Licensed Practical Nurse bringing with her 17 years of experience in disease management and reproductive medicine. After a successful nursing career, Lori attended Camden County Community College where she earned her registered dietitian certificate. Now Lori is Innovative’s latest addition to our workplace wellness team working as...
Read MoreTemporary Safe Harbor for Online Posting of SBCs
A Summary of Benefits and Coverage (SBC) is four-page (double-sided) communication required by the federal government under the Patient Protection and Affordable Care Act (ACA). It must contain specific information, in a specific order and with a minimum size type, about a group health benefit’s coverage and limitations. An SBC...
Read MoreIRS Proposes Minimum Value Rule Change to Mesh IRS and HHS Rules
Beginning in 2015, under the Patient Protection and Affordable Care Act (ACA), large employers must offer affordable, minimum value coverage to their full-time employees or potentially pay a penalty. Some companies have or had been marketing a plan that they state satisfies the minimum value requirement (an actuarial value of...
Read MoreHHS Proposes First of Anticipated Nondiscrimination Regulations
The Department of Health and Human Services (HHS) has issued the first of the anticipated nondiscrimination rules, which sets forth proposed regulations to implement Section 1557 of the Patient Protection and Affordable Care Act (ACA). Section 1557 provides that individuals shall not be excluded from participation, denied the benefits of,...
Read MoreAffordable Care Act Information Returns
Under the Patient Protection and Affordable Care Act (ACA), individuals are required to have health insurance while applicable large employers (ALEs) are required to offer health benefits to their full-time employees. In order for the Internal Revenue Service (IRS) to verify that (1) individuals have the required minimum essential coverage,...
Read More6055 Reporting, HRAs, and “Supplemental Coverage”
The Affordable Care Act (ACA) implemented section 6055 of the Internal Revenue Code, which requires IRS reporting from any entity that provides “minimum essential coverage” (MEC) to individuals. Employers who are applicable large employers (ALEs) have related reporting obligations under section 6056. Beginning in 2013, during the proposed rulemaking stage,...
Read MoreIRS Releases Draft 2015 Instructions for 6055/6056 Reporting
Under the Patient Protection and Affordable Care Act (ACA), individuals are required to have health insurance while applicable large employers (ALEs) are required to offer health benefits to their full-time employees. In order for the Internal Revenue Service (IRS) to verify that (1) individuals have the required minimum essential coverage,...
Read MoreVeterans with TRICARE; VA Coverage Won’t Count Toward Applicable Large Employer Status
The Surface Transportation and Veterans Health Care Choice Improvement Act (STVHCC) of 2015 was signed into law by President Obama on July 31, 2015. The Act, also known as H.R. 3236, is focused on surface transportation programs but affects rules regarding how to count employees under the Patient Protection and...
Read MoreIRS Issues Second Notice to Assist in Developing Cadillac Tax Regulations
The IRS has issued its second notice regarding the upcoming implementation of the Patient Protection and Affordable Care Act’s (ACA) excise tax on high cost employer-sponsored health coverage, also known as the “Cadillac tax.” Beginning in 2018, plans that provide coverage that exceeds a threshold will owe the tax. The...
Read MoreDOL Issues Guidance on Classification of Independent Contractors
The Department of Labor (DOL) has issued an “Administrator’s Interpretation” to assist employers in determining if a worker is an employee or an independent contractor. The DOL has determined that many employers are incorrectly classifying employees as independent contractors, which can harm the worker and open the employer up...
Read MorePreventive Services Final Rules
Federal agencies released final regulations on the preventive services mandate of the Patient Protection and Affordable Care Act (ACA) that requires non-grandfathered group health plans to provide coverage without cost-sharing for specific preventive services, which for women include contraceptive services. After pushback from religious employers, interim final regulations, objections from certain...
Read MoreMid-Size Employers: Transition Relief and Community Rating
The employer shared responsibility (i.e., “play or pay”) requirements went into effect in 2015 for large employers only (those with 100 or more full-time or full-time-equivalent employees). Even though they generally will not be liable for penalties until 2016, mid-size employers (employers with 50 to 99 full-time or full-time-equivalent employees)...
Read MoreInnovative Benefit Planning Principal Mark Sulpizio Sponsors Community Access Unlimited Annual Golf Outing that raises $48,000 for people with disabilities and at-risk youth
Community Access Unlimited is a statewide nonprofit providing support programs and services to more than 6,000 adults with disabilities as well as youth served under the Department of Children and Families (DCF) to enable them to live independently in the community, in areas including vocational and life-skills training, education, advocacy...
Read MoreTrade Bill Increases ACA Reporting Penalties;
Most employers are familiar with the penalties assessed to applicable large employers that fail to offer minimum essential coverage that is minimum value and affordable. In addition to being required to offer coverage, employers (all applicable large employers, and all employers with self-funded plans regardless of size) are required to...
Read MoreU.S. Supreme Court Finds Same Sex Marriage Is Protected by the 14th Amendment
The Supreme Court ruled in Obergefell v Hodges, that the 14th Amendment requires a state to license a marriage between two people of the same sex, and to recognize a marriage between two people of the same sex when their marriage was lawfully licensed and performed out of state. The...
Read MoreTOP FIVE WORTHWHILE WELLNESS APPS–FOR FREE!
1. MyFitnessPal Don’t be a mindless eater! One of the best ways to lose weight and keep it off is to track what you eat and drink throughout the day. Create a profile on MyFitnessPal, enter your weight goal and begin tracking your food intake and physical activity. The app...
Read MoreMid-Size Employers: Transition Relief and Community Rating
The employer shared responsibility (i.e., “play or pay”) requirements went into effect in 2015 for large employers only (those with 100 or more full-time or full-time-equivalent employees). Even though they generally will not be liable for penalties until 2016, mid-size employers (employers with 50 to 99 full-time or full-time-equivalent employees)...
Read MoreIRS Issues Additional FAQs and Hosts Webinar to Assist with Reporting Requirements under PPACA’s Play or Pay
Background In order for the Internal Revenue Service (IRS) to verify that (1) individuals have the required minimum essential coverage, (2) individuals who request premium tax credits are entitled to them, and (3) applicable large employers (ALEs) are meeting their shared responsibility (play or pay) obligations, employers with 50 or...
Read MoreRegion Matters When It Comes to HSA Funding, CDHP Adoption
We’ve already discussed Health Savings Account (HSA) activity at length, looking first at the correlation between generous HSA contributions and increased enrollment in consumer-driven health plans (CDHPs). Second, we looked at how HSAs have performed in recent years across different industries. Now, we’ll look closer at HSA activity across different regions of...
Read MoreTop 5 Questions about Medicare Secondary Payer Rules
Under federal regulations, Medicare is a secondary payer for many individuals who have an employer group health plan available to them, either as an employee or the dependent spouse or child of the employee. Generally the Medicare Secondary Payer rules prohibit employers with more than 20 employees from in any...
Read MorePotential Employer Penalties under the Patient Protection and Affordable Care Act
Employers that do not meet the requirements of the Patient Protection and Affordable Care Act (PPACA) need to be concerned about several potential penalties. Two significant penalties include the excise tax, which can be as much as $100 per affected individual per day, and the penalties that larger employers must...
Read MoreWraparound Excepted Benefits to Launch with Two Pilot Programs
Health plan sponsors would be permitted to offer wraparound coverage to employees purchasing individual health insurance in the private market, including the Marketplace, in limited circumstances, under a new Final Rule issued by the Department of Labor (DOL) and other federal agencies. The Final Rule, published March 18, 2015, sets forth two narrow pilot...
Read MoreIndustry Differences Among Health Savings Accounts
While recent survey data shows that, on average, employers are decreasing the amount they’re willing to contribute to employee Health Savings Accounts (HSAs), there are some industries that have not seen such trends. On average, employees saw a 10 percent decrease in their average single HSA employer contribution from the previous year,...
Read MoreSCOTUS and the Future of U.S. Health Care
The Patient Protection and Affordable Care Act (PPACA), commonly referred to as “Obamacare,” was signed into law with the intention of decreasing the number of uninsured Americans and reducing the overall costs of health care in the United States. In order to increase the number of U.S. citizens covered, a...
Read MoreCongress Taking (Small) Steps for Employee Wellness Programs
The Patient Protection and Affordable Care Act (PPACA) specifically encourages and promotes the expansion of wellness programs in both the individual and group markets. In the individual market, the secretaries of the departments of Health and Human Services (HHS), Treasury, and Labor are directed to establish a pilot program to...
Read MoreCost Sharing Limits Changing for 2016
In the Benefit and Payment Parameters for 2016 Final Rule issued in February 2015, federal agencies included a clarification that annual cost-sharing limitations for self-only coverage apply to all individuals, regardless of whether the individual is covered by a self-only plan or is covered by another kind of plan. Cost sharing refers...
Read MoreSupreme Court Hears Oral Argument in Subsidy Eligibility Battle
On March 4, 2015, the U.S. Supreme Court heard oral arguments in King v. Burwell, a case that centers on the meaning of statutory language in the Patient Protection and Affordable Care Act (PPACA). At question in the case is whether or not the Internal Revenue Service (IRS) may issue regulations...
Read MoreCompliance Recap – March 2015
Coming off a busy February, regulatory agencies were noticeably quiet during the month of March. This allowed the Supreme Court to take the spotlight with oral arguments in the Patient Protection and Affordable Care Act (PPACA) related case, King v. Burwell. A clarifying FAQ was issued regarding cost-sharing limits for...
Read MorePPACA’s Impact on How CDHPs and HSAs Work Together
Employer health savings account (HSA) funding strategies have changed in recent years in response to the Patient Protection and Affordable Care Act (PPACA) and its impact on employer-sponsored health insurance plans. Employers are contributing less, on average, to HSAs and the increase in popularity of cost-saving consumer-driven health plans (CDHPs)...
Read MoreDefinition of “Spouse” Updated for FMLA
The Department of Labor has issued an updated definition for “spouse” under the Family and Medical Leave Act (FMLA) to make compliance with FMLA easier for both employers and employees. The new regulations will be effective on March 27, 2015, and will define “spouse” as a husband or wife, which...
Read MoreFinal Rule Issues Standards for Insurers and Marketplaces in 2016
Recently, the Centers for Medicare and Medicaid Services and the Department of Health and Human Services issued a Final Rule with standards for insurers and Marketplaces in 2016, covering topics such as transparency in health insurance rate increases, formulary drug lists, drug mail order opt out provisions, determination of minimum...
Read MoreGrowing Pains: Why Adolescence Is About To Get That Much Harder
Employers that are growing up, and are in the awkward teenage years, are about to get a big surprise, and not the good kind. When a company first opens, they are excited when they first implement their benefit plans for their handful of employees. They offer one or two medical...
Read MoreIRS Provides Details on Reimbursing Premiums for Individual Health Coverage or Medicare Part B, Part D, or Medigap for Active Employees
On February 18, 2015, the Internal Revenue Service (IRS) issued Notice 2015-17. This Notice addresses employer payment or reimbursement of individual premiums in light of the requirements of the Patient Protection and Affordable Care Act (PPACA). For many years, employers were permitted to reimburse premiums paid for individual coverage on a...
Read MoreAgencies Provide Guidance on Single Benefit Products and Excepted Benefits
On February 13, 2015, the regulatory agencies issued an FAQ on whether supplemental health insurance coverage that provides additional categories of benefits may qualify as supplemental excepted benefits. Many provisions of PPACA do not apply to excepted health benefits. Supplemental excepted benefits are those that are provided under a separate...
Read MoreIRS Requests Input on the Cadillac Tax
Beginning in 2018, plans that provide coverage that exceeds a threshold will owe an excise tax that is frequently referred to as the “Cadillac tax.” The threshold generally will be $10,200 for single benefits and $27,500 for benefits provided to an employee, retiree, or member of a bargaining unit and...
Read MoreThink 2014 tax forms are bad? Here come the 1094 and 1095 for 2015!
Our recent blog reviewed the highlights of the new employer and insurer reporting requirements. The chart below is designed to help you sort out who should use which form, and when: For comprehensive information on coverage requirements, due dates, special circumstances, controlled groups and how to complete the forms—including sample situations—...
Read MoreHighlights of Employer and Insurer Reporting Requirements
The Patient Protection and Affordable Care Act (PPACA) provides that individuals who do not have minimum essential (basic medical) coverage will owe a penalty unless they qualify for an exemption. Employers with 50 or more employees that do not offer affordable, minimum value coverage to their full-time employees also will...
Read MoreThe RFP vs. the Two Step Process — Choosing Group Health Insurance
Many employers look at employee benefits as a commodity, bidding out their plans annually — and who can blame them? Rising health care costs coupled with a challenging economic environment have forced many human resources decision-makers to focus heavily on cost. Organizations of all sizes struggle to find a balance...
Read MoreWhy Buy Group Health Insurance through a Broker?
Employers have a lot of choices when it comes to buying group health insurance, including going directly to a carrier (or one of its agents), buying online, or going through a broker. Direct-to-carrier paths make it more difficult to shop the market across product lines, and buying online can leave...
Read MoreIRS Provides Additional Details on Premium Payment Arrangements
The regulatory agencies have recently issued guidance that may affect employers that have been reimbursing premiums for individual health coverage or Medicare Part B, Part D or Medigap premiums for active employees. In addition, new rules were issued for single benefit supplemental plans, which may affect minimum essential coverage programs...
Read MoreHighlights of Employer and Insurer Reporting Requirements
The Patient Protection and Affordable Care Act (PPACA) provides that individuals who do not have minimum essential (basic medical) coverage will owe a penalty unless they qualify for an exemption. Employers with 50 or more employees that do not offer affordable, minimum value coverage to their full-time employees also will...
Read MoreWill Health Insurance Soon Become Health Memberships?
With the passage of the Patient Protection and Affordable Care Act (PPACA), we saw a number of hospitals and provider groups being bought and merged with larger provider groups. This was done for two reasons. One, in part to make sure that they were able to establish more buying power,...
Read MoreIRS Releases Information and Forms for Satisfying the Individual Mandate and Claiming 2014 Premium Tax Credits
Although employers are not required to offer coverage during 2014, individuals are generally required to have health coverage during 2014 and must report on that coverage through their 2014 federal income tax return. In many cases, the employee will be able to simply state through a “yes/no” question on their...
Read MoreTop 5 Questions About The “Cadillac” Tax
The excise tax on high cost plans (also referred to as the Cadillac tax and the 4980I tax) is scheduled to take effect in 2018. To date, regulations have not been issued, so many of the details about how the tax will operate are unclear. (The regulatory agencies are responsible...
Read MoreProposed Changes to Summary of Benefits and Coverage (SBC)
The Department of Labor (DOL), the Department of Health and Human Services (HHS), and the Internal Revenue Service (IRS) have issued proposed regulations that would update the summary of benefits and coverage (SBC) requirement, including the SBC template, instructions, example calculator, and uniform glossary. If adopted, the revised form would be used...
Read MoreInnovative Principal Speaks at Federal Reserve Bank
On Tuesday, January 13th Innovative’s Principal, Mark Sulpizio, was invited to participate at the Entrepreneurs’ Forum of Greater Philadelphia event at The Federal Reserve Bank of Philadelphia. Mark was featured as one of five panelists invited to speak at the EFGP Advisory Boards networking event. The group discussed important topics...
Read MoreInnovative Investment Fiduciaries Presents to HR Association
On Thursday, January 8th, Innovative’s Matthew Bernstein, Retirement Plan Consultant, and Mark Sulpizio, Managing Partner, were asked to speak at the Greater Princeton Human Resources Association’s (GPHRA) monthly meeting in Princeton, New Jersey. The presentation discussed the Pension Protection Act’s plan restatement requirement due April 30th 2016 which requires most...
Read MoreEmployees Just Don’t Understand…
Or are employers just not communicating effectively? In 2015, most organizations have employees that include Baby Boomers, Generation X, Generation Y, and Millennials. Each of these generations is different in the way they find information, digest information, and act on information. Now if you read the title to this post...
Read MoreConsider a Wellness Coach
Biometric testing has become the latest rage in wellness programs. If you’re unfamiliar with this, biometric testing (sometimes called biometric screening) involves measuring employees’ blood pressure, blood glucose, cholesterol, and similar measurements of employees’ health status. This testing can be a very helpful and important part of a corporate wellness...
Read MoreAre You Benchmarking Your Health Plan Correctly?
Many employers benchmark their health plans against other employers with the same carrier or using nationally available data. But the benchmarking best practice is to compare your plan with others based on plan type, region, employee size, and industry. Without this more granular data, you could be missing key data...
Read MoreDetermining Minimum Value and Affordability
The IRS has released final regulations that address how wellness incentives or penalties, contributions to a health reimbursement arrangement, and employer contributions to a Section 125 plan are applied to determine affordability. While these regulations were issued in connection with the individual shared responsibility requirement (also called the individual mandate),...
Read More2015 Cost-of-Living Adjustments
Many employee benefit limits are automatically adjusted each year for inflation (this is often referred to as an “indexed” limit). The Internal Revenue Service and the Social Security Administration have released a number of indexed figures for 2015. Limits of particular interest to employers include the following. For health and...
Read MoreSupreme Court Agrees to Rule on Availability of Premium Tax Credits
Premium tax credits are only available to individuals who obtain health coverage through a Marketplace. A dispute has arisen as to whether the IRS has the ability to interpret PPACA to allow the subsidy to individuals who obtain coverage through any Marketplace, or whether the language of PPACA limits eligibility...
Read MoreUBA Releases 2014 Health Plan Survey Executive Summary
Recent survey data from the 2014 United Benefit Advisors Health Plan Survey, the nation’s largest health plan survey, shows that employers continue to shift a greater share of expenses to employees through out-of-pocket cost increases and reductions in family benefits, as well as delay many effects of the Patient Protection and...
Read MoreThe “Play or Pay” Package
The employer-shared responsibility (“play or pay”) requirements do not apply to small employers and have been delayed until 2016 for employers with 50-99 employees. This raises the question – what exactly is included in the play or pay requirement, which a small employer may be able to ignore and that...
Read MoreDecember Wellness Newsletter
QuickBites Weight-Loss Winners The National Weight Control Registry (NWCR) studies people who have lost at least 30 pounds and kept it off for a year or longer. More than 10,000 people have enrolled in the study. Once a year, members answer questions about their weight, diet, and exercise habits. The...
Read MoreCompliance Recap – November 2014
The month of November brought a new delay in reporting required from self-funded plans. It also brought several new notices and regulations that may affect sponsors of group health plans and an updated employer guide and health plan compliance checklist from the Department of Labor (DOL). Transitional Reinsurance Program Filing...
Read MoreWellness While Away
We all have barriers that get in the way of leading healthy lives. As we enter the holiday season, they seem to pile up more and more. My colleagues in the office will be the first to tell you, willpower is not one of my strengths when it comes to...
Read MoreTransitional Reinsurance Fee Filing Date Extended to December 5
The Centers for Medicare and Medicaid Services (CMS) has extended the deadline for group health plans to complete their 2014 transitional reinsurance fee (TRF) submission. The announcement, which was released late on November 14, 2014, states that the filing is now due by 11:59 p.m. on Friday December 5, 2014....
Read MoreThe Benefit Guardian Makes an Appearance at Halloween
This past Halloween we were honored to see the first ever Innovative Benefit Guardian costume from one of our very own clients. David Liero, an employee from AFS, designed and assembled his one of a kind Benefit Guardian costume. David told us, “I first got the idea for the costume...
Read MoreCOMPLIANCE ALERT: Premium Reimbursement Arrangements
The Department of Labor (DOL) has just published a series of FAQs regarding premium reimbursement arrangements. Specifically, the FAQs address the following arrangements: An arrangement in which an employer offers an employee cash to reimburse the purchase of an individual market policy. Where an employer provides cash reimbursement for the...
Read MoreSubstance Abuse and Teens: Strategies for Prevention
Every year since 1975, the Monitoring the Future study has measured drug, alcohol and cigarette use among American youth. The study, sponsored by the National Institute on Drug Abuse (NIDA), surveys more than 40,000 eighth, tenth and twelfth graders. The 2013 results show a decrease in tobacco and alcohol use...
Read More2015 Cost-of-Living Adjustments
The IRS has issued the cost-of-living adjusted figures for qualified plans and for several fringe benefits for 2015. Of particular interest to many employers are: • An increase in the maximum employee contribution to a health flexible spending account (HFSA) to $2,550 • An increase in the 401(k) and 403(b)...
Read MoreRequirement to Obtain a Health Plan Identifier (HPID) Delayed
On Friday October 31, 2014 the Department of Health and Human Services (HHS) quietly updated its Health Plan Identifier information page to delay the requirement that insurance carriers and self-funded health plans obtain a health plan identifier (HPID). The delay is in effect until further notice. Plans that have already...
Read MoreHighlights of Wellness Program Requirements
The wellness program rules provide an exception to the general rule that employers may not take a person’s health status into account with respect to eligibility, benefits, or premiums under a group health plan. Wellness programs, therefore, are allowed if they are designed to help employees improve their health; if...
Read MoreFrequently Asked Questions about Grandfathered Plans
As employers determine their plan designs for the coming year, those with grandfathered status need to decide if maintaining grandfathered status is their best option. Innovative, in conjunction with our Partner firm United Benefit Advisors, has created an FAQ to address the questions employers have about grandfathering a group health...
Read MoreEssential Health Benefits, Minimum Essential Coverage, Minimum Value Coverage – What’s The Difference?
The Patient Protection and Affordable Care Act (PPACA) uses terms that sound alike for three very different things. Here’s a closer look at these terms, and when they’re used. Essential Health Benefits Significantly affects individuals and small employers with a fully insured plan. Has a limited impact on self-funded and...
Read MoreUpdate: Same-Sex Marriages and Group Health Benefits
On October 6, 2014, the Supreme Court of the United States declined to review seven cases in which the lower appeals court had ruled that a state law or constitutional provision that prohibited same-sex marriage was unconstitutional. This declination means that the ruling of the appeals court is law, and...
Read MoreCompliance Alert! Deadline Approaching for Larger Self-Funded Health Plans To Obtain a Health Plan Identifier Number
To meet federal requirements, large health plans must obtain a national health plan identifier number (HPID) by November 5, 2014. For this requirement, a large health plan is one with more than $5 million in annual receipts. The Department of Health and Human Services (HHS) has said that since health...
Read MoreSkinny Plans and Minimum Value: Do these plans really pass the test?
There is a lot of buzz in the market right now as employers are implementing their plans for the upcoming year. Many employers are looking at ways to keep their costs for medical coverage low, but still meet the requirements of the Patient Protection and Affordable Care Act (PPACA). These...
Read MoreDON’T FORGET TO REGISTER! Philadelphia Lunch ‘N Learn this Friday
Are your employees getting their fair share? In 2012, the DOL issued new disclosure regulations requiring service providers to disclose the services provided and fees charged to retirement plans. Recently, the DOL has commented that the new regulations have not produced the desired effect, that plan sponsors review the disclosures...
Read MoreIRS Notice Addresses Handling of Changes in Measurement and Stability Periods
Large employers (for 2015, this generally means those with 100 or more full-time or full-time equivalent employees) may use either the monthly or look-back method to determine whether an employee on average works 30 or more hours per week, and for whom a penalty may be owed if adequate health...
Read MoreExcepted Benefits – “Limited Scope” Dental and Vision Plans and EAPs
On September 26, 2014, the U.S. Department of Health and Human Services (HHS), the Internal Revenue Service (IRS), and the Department of Labor (DOL) released final regulations that explain when dental and vision plans and employee assistance plans (EAPs) will be considered “excepted benefits.” Excepted benefits are health benefits that are...
Read MoreIRS Allows Additional Section 125 Change in Status Events
On September 18, 2014, the Internal Revenue Service (IRS) issued Notice 2014-55 which allows employers to amend their Section 125 plans to recognize several new changes in status events. Open Enrollment in the Health Insurance Marketplace Prior to this new notice, an opportunity to enroll in the health insurance Marketplace (or...
Read MoreOur September Educational Events were a Tremendous Success!
Our Innovative team presented an educational seminar at DelFrisco’s Double Eagle Steakhouse in Philadelphia on September 19th, and also at Fleming’s Steakhouse in Marlton on September 25th. The events, which introduced innovative solutions for controlling the costs within your health plan while complying with PPACA, attracted C-level executives as well...
Read MoreIRS Issues Drafts of Instructions for Employer and Individual Responsibility Reporting Forms
The following is a summary of draft instructions. Some of this information may change when the final forms and instructions are released. In order for the Internal Revenue Service (IRS) to verify that individuals have the required minimum essential coverage, individuals who request premium tax credits are entitled to them,...
Read MoreInnovative Investment Fiduciaries Guest Presenters
On Tuesday, September 16th, Innovative’s Matthew Bernstein, Qualified Plan Consultant, and Mark Sulpizio, Managing Partner were asked to speak at MID Jersey Chamber of Commerce’s quarterly NPEC (Non-Profit Executive Council) meeting in Hamilton New Jersey. The presentation focused on the impact of the Department of Labor’s 408(b)(2) qualified plan fee...
Read MoreFrequently Asked Questions about the Transitional Reinsurance Fee (TRF)
The transitional reinsurance fee (TRF) applies to fully insured and self-funded major medical plans for 2014, 2015, and 2016. The purpose of the fee is to provide funds to help stabilize premiums in the individual insurance market in view of uncertainty about how the Patient Protection and Affordable Care Act...
Read MoreEating For Healthy Cholesterol
Cholesterol The American Heart Association estimates that more than 120 million Americans have unhealthy cholesterol levels, putting them at greater risk for heart attack and stroke. Cholesterol is found in every cell in your body. When there’s too much cholesterol in your blood, you may develop fatty deposits in...
Read MoreGroup Health Plan Notices: What Do You Need To Include?
Employers that sponsor group health plans are required to give eligible employees a number of notices each year. Some notices must be given by a particular date, and some must be given as part of the enrollment packet. (This means that non-calendar year plans may need to provide Medicare Part...
Read MoreHighlights of the Summary of Benefits and Coverage Requirement
Plan administrators of group health plans, which includes all employers regardless of size or type of business with the exception of those that have been grandfathered, must provide a Summary of Benefits and Coverage (SBC) to eligible individuals. This requirement applies primarily to medical (PPO, HDHP, HMO, etc…) coverage. There...
Read MoreHow Can You Help Reduce Air Pollution?
Environmental Health Works Both Ways This month we look at how the environment affects health. Knowing about health problems related to the environment is an important part of making healthy lifestyle choices. This awareness starts at home. A safe, healthy environment in the home includes: Avoiding lead Testing for radon...
Read MoreIRS Issues Drafts of Individual Responsibility Reporting Forms
The following is a summary of draft forms. Some of this information may change when final forms, and the instructions, are released. In order for the IRS to verify that individuals and employers are meeting their shared responsibility obligations, and that individuals who request premium tax credits are entitled to...
Read MoreA September Lunch Event Is On The Calendar!
On February 10, 2014, the IRS issued final regulations on the employer requirements, often known as “Play or Pay.” For some employers Play or Pay is delayed until 2016, for others, compliance is still required in 2015. Make sure you know where you stand. Please join us on Friday September...
Read MoreCost of Living Adjustments for 2015
Many of the thresholds in PPACA have annual cost-of-living adjustments. The IRS has released the 2015 “affordability” thresholds. Affordability is measured differently for purposes of eligibility for the premium tax credit/subsidy (and any employer-shared responsibility penalty triggered by an employee receiving a premium subsidy) and the individual-shared responsibility penalty. For...
Read MoreCourts Issue Opposite Rulings in PPACA Subsidies Cases
On July 22, 2014, two Courts of Appeals issued decisions that address whether only people who live in states that have state-run Marketplaces (which are also called exchanges) are eligible to receive premium tax credits or subsidies under the Patient Protection and Affordable Care Act (PPACA). One court held that...
Read MoreAdditional Rules on Contraceptive Coverage
Following up on the Supreme Court’s decision in the Hobby Lobby case, the Departments of Labor, Health and Human Services, and Treasury have issued an FAQ that reminds employers that ERISA requires that plan participants be advised of a material reduction in benefits within 60 days after the reduction becomes effective....
Read MoreWill Your Private Plan Owe an MLR Rebate This Year?
MLR Rebate Considerations – Private Plans As was the case last year, insurers with medical loss ratios (MLRs) that were below the prescribed levels on their blocks of business must issue rebates to policyholders. Insurers must pay rebates owed on calendar year 2013 experience by August 1, 2014. The rules...
Read MoreWill Your Government or Church Plan Owe an MLR Rebate This Year?
MLR Rebate Considerations – Government and Church Plans As was the case last year, insurers with medical loss ratios (MLRs) that were below the prescribed levels on their blocks of business must issue rebates to policyholders. Insurers must pay rebates owed on calendar year 2013 experience by August 1, 2014....
Read MoreThe Federal Court of Appeals Says Subsidies for Obamacare are Illegal!
After an in-depth, careful reading of the Affordable Care Act, the Federal Appeals Court panel ruled 2-1 that government subsidies used to purchase health insurance on HealthCare.gov are illegal. The ruling stated that only exchanges that are run by an individual state, or the District of Columbia, are permitted to...
Read MoreFourth Circuit Court Says Subsidies in the Federal Exchange Are Legal
We now have a decision from another Court of Appeals (this time it’s the Fourth Circuit) on the exact same subsidy issue as posted earlier today. This court has held that it is legal for individuals enrolled in federally-run exchanges to receive subsidies. If this decision ultimately prevails, employers would...
Read MoreWhy HSAs Linked to HDHPs are Making a Comeback
According to new information from United Benefit Advisors (UBA), health savings accounts (HSAs) are outpacing health reimbursement arrangements (HRAs) in both adoption and participation rates. And now that metal tier health plans [e.g., platinum, gold, silver, etc.] are allowed higher deductibles, employers are increasingly looking at HSA qualified plans for...
Read MoreFollow-Up to the Hobby Lobby Decision
The Supreme Court of the United States recently decided in a case generally referred to as the Hobby Lobby case that closely-held corporations whose owners have religious objections to providing coverage for contraceptives are not required to provide that coverage to satisfy PPACA requirements. We still do not know how...
Read MoreWhat Does July 31st Mean To You?
Form 5500 With the exception of government plans (including most public schools) and many church plans which are exempt, plans on a calendar year that must comply with ERISA must file Form 5500 by July 31st. This form is part of ERISA’s overall reporting and disclosure framework, which is intended...
Read MoreGet Active for Summer!
People who are physically active live longer and have a lower risk for chronic disease. Going outdoors for exercise is good for your mental and physical well-being. Recent studies have found that, compared with exercising indoors, exercising in natural environments made people feel revitalized and energetic. The CDC advises adults...
Read MoreHave You Registered for Our July 15th Lunch Event in Cherry Hill?
Are your employees getting their fair share? In 2012, the DOL issued new disclosure regulations requiring service providers to disclose the services provided and fees charged to retirement plans. Recently, the DOL has commented that the new regulations have not produced the desired effect, that plan sponsors review the disclosures...
Read MoreWhat Employers Need to Know about SCOTUS Hobby Lobby Ruling
On June 30, 2014 the U.S. Supreme Court issued a decision in a case generally referred to as the Hobby Lobby case. Hobby Lobby is a family-owned for-profit corporation. The family that owns Hobby Lobby strongly believes that it would violate their deeply held religious values and obligations to provide...
Read MoreInnovative Receives Rave Reviews Once Again!
Last Friday at Sullivan’s Steak House in King of Prussia, our Innovative team revealed the three greatest concerns of our market regarding PPACA at an educational seminar lunch event. In speaking with clients and other employers in the area, it became clear that guidance is needed not only on compliance,...
Read MoreHow Does the New Orientation Period Affect the 90-Day Waiting Period?
The DOL recently (June 25, 2014) issued additional regulations regarding an Orientation Period for Employers. This Orientation Period is meant to provide both employer and employees alike the opportunity to evaluate whether the employment situation is satisfactory for each party. This period can occur prior to the start of the maximum...
Read MoreThe New Jersey Athletic Conference Board Invites Innovative As Their First Guest Speaker!
On Wednesday June 18th, Innovative’s Ryan Kastner, Employee Benefits Consultant, and Scott Agostini, Managing Director, were invited to speak at the NJAC (New Jersey Athletic Conference) semi-annual Board of Athletic Directors meeting in Atlantic City, where they educated the attendees on the possible effects of Health Care Reform to their...
Read MoreWhat Are The Final Regulations For PPACA’s Mandatory Reporting?
On September 5, 2013, the IRS issued proposed rules implementing the information reporting requirements under Code Sections 6056 and 6055. These proposed rules reflected a potential massive and duplicative amount of paperwork required by employers to comply with the reporting requirements of PPACA. On March 10, 2014, the IRS issued...
Read MoreNew Model COBRA Notices Should Be Used By Employers
The Department of Labor has published new model COBRA notices that reflect that coverage is available in the public health insurance exchanges and include information on special enrollment rights. Key points: • Employers should utilize the revised model notices. • Employers should be proactive in communicating with employees about “Marketplace”...
Read MoreSummer Skin Care Myths and Facts
Your skin is one hard-working organ. (Yes, it is considered an organ. In fact, it’s the body’s largest!) Skin acts as a protective barrier between your internal organs and the outside world. It’s a busy communications hub, constantly updating info on touch and temperature, and passing that info along to...
Read MoreHighlights of the Patient Centered Outcomes (PCORI) Comparative Effectiveness Fee
Updated June 2014 The Patient-Centered Outcomes Research Institute (PCORI) fee applies from 2012 to 2019. The fee is due based on plan/policy years ending on or after October 1, 2012, and before October 1, 2019. The fee is due by July 31 of the year following the calendar year in...
Read MoreDon’t Miss Our Next Seminar Lunch Event in King of Prussia!
PPACA Strategies- Innovative Solutions to Control Your Bottom Line With the passing of the Patient Protection and Affordable Care Act, CEO’s and CFO’s have never paid more attention to employee benefits than they are now. Please take advantage of the opportunity to be the most informed person in the room!...
Read MoreDo You Have The Correct Form To File Your PCORI Fees?
The Patient-Centered Outcomes Research Institute (PCORI) fee is imposed on insurers and plan sponsors of self-insured group health plans, with plan years ending after September 30, 2012 and before October 1, 2019. Sponsors of calendar year plans are required to pay the annual fee by July 31 of each year...
Read MoreAre The Fees In Your Retirement Plan Reasonable?
Are your employees getting their fair share? In 2012, the DOL issued new disclosure regulations requiring service providers to disclose the services provided and fees charged to retirement plans. Recently, the DOL has commented that the new regulations have not produced the desired effect, that plan sponsors review the disclosures...
Read MoreSearching For Answers? Find Out How Your Company Compares
Don’t Miss Your Chance To Participate In The Largest Health Plan Benchmarking Survey In The Country! End your search for answers by participating in the 2014 UBA Health Plan Benchmarking Survey…and you will automatically be entered in a raffle to win the new iPad Air!!! Your survey needs to be...
Read MoreCOMPLIANCE ALERT! Self-Funded Health Plans Must Obtain a Health Plan Identifier Number
To meet federal requirements large health plans must obtain a national health plan identifier number (HPID) by November 5, 2014. For this requirement, a large health plan is one with more than $5 million in annual receipts. The Department of Health and Human Services (HHS) has said that since health...
Read MoreHow Does COBRA Affect Marketplace Enrollment?
The Obama Administration announced last week that workers who are eligible to continue health insurance coverage through COBRA (Consolidated Omnibus Budget Reconciliation Act), will now have the option of purchasing a plan through the Health Insurance Marketplace without having to wait until open enrollment. In many cases, workers will be...
Read MoreJoin Us For Our Lunch ‘N Learn May 16th: Managing Benefit Costs In The Health Care Reform Era
On February 10, 2014, the IRS issued final regulations on the employer-shared responsibility requirements, often known as “Play or Pay.” For some employers Play or Pay is delayed until 2016, for others, compliance is still required in 2015. Where do you stand? Please join us for a sizzling lunch where...
Read MoreInnovative Exhibits at the 28th Annual Tri-State HRMA Conference!
It was a “hole-in-one” day at the Westin in Mount Laurel on May 1st where about 250 attendees, and numerous exhibitors, came together for a day of education, networking and fun! Innovative Consultants Ryan Kastner, Dan Foley and Matt Bernstein, along with our Managing Director Scott Agostini, challenged attendees to...
Read MoreUnderstanding Arthritis
Understanding Arthritis More than one in five adult Americans has some form of arthritis. Arthritis causes pain, stiffness and limited movement in affected joints. There are at least 100 different types of arthritis. The two most common forms are osteoarthritis and rheumatoid arthritis. Exercise is a valuable tool for managing...
Read MoreCongratulations to Maria Black!
Time flies when you’re having fun! Maria Black is celebrating 13 years with Innovative Benefit Planning this month! As a Senior Account Manager, Maria works diligently with her clients on designing and administering their employee benefit packages. Maria’s clients love and appreciate her, as evidenced by the frequent “Wows!” that...
Read MoreInnovative Consultant, Ryan Kastner, Advises PEBA Attendees on Managing Benefit Costs
The 32nd Annual PEBA Forum took place last Thursday April 24th at the Hilton on City Line Avenue in Philadelphia. Innovative was proud to be an Exhibitor at this event and arrived ready to encourage attendees to take a chance at our mini golf game in order to win a...
Read MoreOur Innovative Team Continues To Grow With Scott Agostini As Managing Director!
We are very excited to announce the addition of Scott Agostini to Innovative Benefit Planning. As Managing Director, Scott will provide oversight on the day-to-day business operations. In addition, Agostini will use his many years of Human Resources management experience to grow Innovative’s HR consulting practice. Most recently, Agostini was...
Read MoreCost-Of-Living Adjustments for Health Savings Accounts (HSAs)
The IRS has issued the 2015 cost-of-living and coverage adjustments for HSAs. All limits have increased for 2015 as follows: Annual contribution limitation: Individual $3,350 (up from $3,300) Family $6,650 (up from $6,550) Annual Maximum Out-Of-Pocket Limits for HDHP*: Individual $6,450 (up from $6,350) Family $12,900 (up from $12,700) Annual...
Read MoreInnovative’s Mark Sulpizio Is Quoted In Employee Benefit Advisors
In the last few years, executive level employees have made a shift from working for larger companies, to running smaller companies. However, the benefits typically available at smaller companies can’t compare with those of their larger counterparts. So what is an employer to do in order to attract and retain...
Read MoreProposed Regulation: Health Plans Participating in the Exchange Must Provide a 90-Day Grace Period for Subsidized Coverage
For those individuals that purchase a subsidized health insurance plan through the Exchange, and have previously paid at least one full month’s premium during the benefit year, the insurance plan must provide for a 90-day grace period for premium payment before canceling for non-payment. Within this 90-day period, claims for...
Read MoreJoin Us At The 32nd Annual PEBA Forum On April 24th!
Innovative is looking forward to being an exhibitor at the 32nd Annual PEBA (PennJerDel Employee Benefits & Compensation Association) Forum this month, on Thursday April 24, 2014. The event will take place at the Hilton on City Line Avenue and is expecting an attendance of more than 300 compensation, benefit...
Read MoreHow Fit Are You?
Fat or Fit? Being healthy and fit is not just about being thin. Managing health is important for everyone, no matter what their size or shape. Not smoking, eating a healthy diet and managing stress are all vital to good health. Regular physical activity greatly reduces health risks too, even...
Read MoreJoin Us May 9th For Our Princeton Lunch ‘N Learn: Are The Fees In Your Retirement Plan Reasonable?
_ Are your employees getting their fair share? _ In 2012, the DOL issued new disclosure regulations requiring service providers to disclose the services provided and fees charged to retirement plans. Recently, the DOL has commented that the new regulations have not produced the desired effect, that plan sponsors review...
Read MoreRegulation Update: House Votes Full-Time As 40 Hours!
In a House vote of 248 to 179 last Thursday, the definition of full-time employee under The Patient Protection and Affordable Care Act (PPACA) was changed from 30 hours per week back to 40 hours per week. The bill was sponsored by Rep Todd C. Young, a Republican from Indiana. ...
Read MoreLook Who’s In The News!
Terriann Procida, one of Innovative’s Founding Partners, is once again recognized by the local community for her charitable contributions. Her work as Chairperson for the Samaritan Healthcare & Hospice Annual Gala for three years was recognized at the 2014 Gala by awarding her the Samaritan Circle of Excellence Award. In...
Read MoreSearching For Answers? Find Out How Your Company Compares
Don’t Miss Your Chance To Participate In The Largest Health Plan Benchmarking Survey In The Country! End your search for answers by participating in the 2014 UBA Health Plan Benchmarking Survey…and you will automatically be entered in a raffle to win the new iPad Air!!! Your survey needs to be...
Read MoreInnovative Welcomes Two New Team Members!
We are happy to announce the addition of two new members to the Innovative team: Molly Greer and Jennifer Fitzwater! Molly Greer is a return employee to Innovative after a 13 year respite. Molly’s previous experience in eligibility and claims has allowed a seamless transition back to Innovative. Molly is...
Read MoreMarketplace Enrollment Deadline Is Delayed For Some
The March 31, 2014 deadline for enrolling in the Marketplace is less than a week away, but for those who have at least started the enrollment process by that deadline, there will not be a penalty for an incomplete application. According to the U.S. Department of Health and Human Services,...
Read MoreOrganics is a growing industry in the United States
Organics is a growing industry in the United States. This is especially apparent in the produce aisle. Today, nearly all supermarkets offer a variety of organically grown fruits and vegetables. Sales of organic produce in 2013 increased by 12% over 2012 sales. In fact, 35¢ of every dollar spent on...
Read MoreIRS Releases Final Reporting Regulations
In order for the Internal Revenue Service (IRS) to verify that individuals and employers are meeting their shared responsibility obligations and that individuals who request premium tax credits are entitled to them, employers and issuers will be required to provide reporting on the health coverage they offer. The reporting requirements...
Read MoreOption for Some to Renew Policies That Do Not Fully Meet PPACA Standards
On March 5, 2014, the Department of Health and Human Services (HHS) released a Bulletin that allows state insurance departments to permit the renewal through October 1, 2016, of individual and small group policies that do not meet the “market reform” requirements of the Patient Protection and Affordable Care Act...
Read MoreThe Deadline Is Just A Few Weeks Away…
The Individual Mandate went into effect January 1, 2014. Compliance for this mandate requires that non-exempt U.S. citizens and legal residents must purchase and maintain “minimum essential coverage” which includes: • Individual market plans offered within a state, whether through or outside the Exchange • Eligible employer-sponsored plans • ...
Read MoreIt Was A Busy Month At Innovative With Two Outstanding Lunch Events and a Gala!
We did not let the snow get in our way in February! The month started off with _ Mark Sulpizio, Innovative Investment Fiduciaries, LLC Principal _, guiding attendees through the Retirement Fee Disclosure Regulations that went into effect in 2012 at a fantastic Seminar Lunch Event at McCormick & Schmick’s...
Read MoreDon’t Miss Your Chance To Participate In The Largest Health Plan Benchmarking Survey In The Country!
End your search for answers by participating in the 2014 UBA Health Plan Benchmarking Survey…and you will automatically be entered in a raffle to win the new iPad Air!!! With close to 11,000 employers participating in 2013, Innovative Benefit Planning, in conjunction with United Benefit Advisors (UBA), annually conducts the...
Read MoreFinal Regulations Issued on Eligibility Waiting Periods
On February 20, 2014, the Department of Health and Human Services (HHS), the Department of Labor (DOL) and the Internal Revenue Service (IRS) released final regulations on the eligibility waiting period requirements. The Patient Protection and Affordable Care Act (PPACA) provides that plans may not require an employee who is...
Read MoreFinal Regulations on Play or Pay: Non-Calendar Year Plans and Next Steps for Employers
Non-Calendar Year Plans Large employers with non-calendar year plans do not have to provide coverage until the start of the 2015 plan year, but the plan year effective date applies only if they meet a number of requirements. The most significant of these are: The employer had a group health...
Read MoreFinal Regulations on Play or Pay: Large Employer Responsibilities and Potential Penalties
If an employer is large enough for the play or pay requirements to apply (100 or more full-time or full-time equivalent employees for 2015 and 50 or more full-time or full-time equivalent employees for 2016 and beyond), two separate requirements, and potential penalties, apply. Full-time continues to mean 30 or...
Read MoreFinal Regulations on Play or Pay: Delay for Some Employers, and Who Is “Large”?
On February 10, 2014, the IRS issued final regulations on the employer-shared responsibility requirements, often known as “play or pay.” This is the requirement that large employers offer adequate coverage to their full-time employees or pay penalties. The final regulations follow the proposed regulations (which were issued in January 2013)...
Read MoreCompliance Alert! Employer Mandate Delayed For Some Employers
The Obama administration announced Monday February 10, 2014 yet another delay in the Employer Mandate portion of PPACA. The first delay pushed the requirement back to 2015 for all “large” employers, meaning those with over 50 employees. This new delay states that companies with 50-99 employees will not have to...
Read MoreWhat Is The DASH Diet?
The DASH diet is a healthy eating plan based on the research studies: Dietary Approaches to Stop Hypertension. The diet has been proven in National Institutes of Health research to help lower your risk of heart disease by lowering blood pressure and lowering cholesterol. Blood pressure control with the DASH...
Read MoreCongratulations to Dan Foley and Ryan Kastner!
A key component of Innovative’s 2014 Strategic Plan is Focusing on improving Ourselves, Client situations and Innovative (FOCI). Dan Foley and Ryan Kastner embraced the initiative of self-improvement by completing the 13 modules of training classes and passing a rigorous examination to earn the designation of Certified Corporate Wellness Specialist®...
Read MoreThe 2014 UBA Health Plan Benchmarking Survey Is Open!
End your search for answers by participating in the 2014 UBA Health Plan Benchmarking Survey…and you will automatically be entered in a raffle to win the new iPad Air!!! With close to 11,000 employers participating in 2013, Innovative Benefit Planning, in conjunction with United Benefit Advisors (UBA), annually conducts the...
Read More2014 Federal Poverty Level Numbers Released by the HHS
The 2014 FPL guidelines have been released and are available here: Federal Register, Volume 79 Issue 14 (Wednesday, January 22, 2014). For employer purposes, they matter primary because eligibility for the premium subsidy is based on FPL. The FPL is up 1.5% over last year. The level for a household...
Read MoreWellness Program Clarifications: Tobacco and Outcome-Based Alternatives
Additional PPACA clarifications were released by the HHS and DOL on January 9, 2014 through an FAQ. Here are the updates you need to know concerning your Wellness Program: Wellness Programs The FAQ states that a plan that offers an annual opportunity to receive an incentive for non-use of tobacco...
Read MorePPACA Update: Mental Health And Substance Abuse
A recent FAQ was released by the DOL and HHS to clarify certain regulations within PPACA. Here is the update on mental health and substance abuse disorders: Mental Health and Substance Abuse Disorders Coverage for mental health and substance use disorder services are an EHB, so non-grandfathered individual and small...
Read MorePPACA Update: Expatriate Plans, Fixed Indemnity Policies (Individual Market) and Volunteer Firefighters
Recent clarifications became available from the HHS and DOL regarding several PPACA regulations. Below are the updates for Expatriate Plans, Fixed Indemnity Policies, and Volunteer Firefighters. Expatriate Plans Insured expatriate plans do not need to comply with most PPACA provisions. The FAQ clarifies that a plan is considered an insured...
Read MoreNew Update To Coverage Under “Preventive Care”
On January 9, 2014, the Department of Health and Human Services (HHS), the Department of Labor (DOL) and the Department of the Treasury (IRS) issued clarification on several outstanding issues within PPACA through an FAQ. Here is what is new for preventive care: Preventive Care The requirement that non-grandfathered plans...
Read MoreNew Clarifications On Out-of-Pocket Maximums Under PPACA
On January 9, 2014 the HHS and DOL issued a new FAQ that addressed issues outstanding under PPACA. Here is the update for out-of-pocket maximums: Out-of-Pocket Limits The FAQ clarifies that, for non-grandfathered plans, the out-of-pocket maximum: Must include deductibles, coinsurance and copayments for essential health benefits (EHBs). A plan...
Read MoreDo You Know When To Use A Wrap Around Plan Document Or Wrap Around SPD?
The Employee Retirement Income Security Act of 1974 (ERISA) regulates employee pension plans and welfare benefit plans, with the exception of government and church plans. It is required by ERISA that plan sponsors describe the terms and conditions of its welfare benefit plans on an official written plan document that...
Read MoreDo You Have Questions About Eligibility Waiting Periods? You Are Not Alone!
The 90-day maximum for eligibility waiting periods is effective as of the start of the 2014 plan year. As employers are beginning to implement this new requirement, many have questions. Together with United Benefit Advisors (UBA), we have created a PPACA Advisor that addresses a number of recurring questions about...
Read MoreTerriann Procida To Receive The “Samaritan Circle of Excellence Award”
We are so proud to announce that Innovative’s Co-Founder, Terriann Procida, will be receiving the “Samaritan Circle of Excellence Award” at this year’s Samaritan Healthcare & Hospice Annual Fundraising Gala in February. The award will be presented to Terriann for her outstanding leadership and dedicated volunteer service to promoting comfort,...
Read MoreW-2 Reporting in 2014: Do You Have To Report Your Health Plan Costs, Or Not?
Employers that issued 250 or more W-2s in 2012 will need to include the cost of health coverage provided to an employee during 2013 on the employee’s W-2. Unlike most PPACA requirements, the 250 W-2 threshold is based on each employer’s situation, not the entire controlled group. The rules have...
Read MoreWhat Are Excepted Benefits?
“Excepted benefits” are health benefits that are limited in some way, such as stand-alone dental, long-term care, hospital indemnity, and Medicare supplement policies. Excepted benefits do not need to meet all of the PPACA requirements and they are not considered “minimum essential” benefits. The agencies have proposed three changes to...
Read MoreWho Will Be Paying An Additional Medicare Tax?
The IRS issued final regulations on the additional 0.9 percent Medicare tax owed by high earners beginning in 2013. Employers must withhold this additional 0.9 percent from the employee’s pay only (there is no employer “match”) once the employee’s pay exceeds $200,000. If you would like a White Paper on...
Read MoreWhat are the Projected 2015 Figures ?
HHS and the IRS released anticipated 2015 figures, including: A transitional reinsurance fee (TRF) of $44 (down from $63 for 2014) Maximum out-of-pocket (OOP) expenses of $6,750 for single coverage and $13,500 for family coverage (up from $6,350 and 12,700 respectively for 2014) A deductible maximum in the small group...
Read More5 Easy Strategies for Coping with Stress
Stress is a fact of life. A little stress can make you feel energized. It may even help you get things done. But constant stress can take a toll on your health. The effect can be both physical and mental. Poorly managed stress is a factor in many chronic health...
Read MoreFrequently Asked Questions About The W-2 Reporting Requirement
Employers that issued 250 or more W-2s in the prior calendar year must include the value of “employer-sponsored group health coverage” on their employees’ W-2s. This means that an employer that issued 250 or more W-2s during 2012 must include the value of employer-sponsored coverage on the employee’s 2013 W-2...
Read MoreWho Is Eligible For The Small Business Tax Credit?
Beginning in 2014, the small business tax credit will only be available to small employers that offer coverage through the SHOP marketplace. Several counties in Washington and Wisconsin will not have SHOPs available in 2014, however. In Notice 2014-6, the IRS states that employers located in those counties will still...
Read MorePre-Existing Condition Insurance Plan Extended
HHS has announced that the Pre-Existing Condition Insurance Plan (PCIP) also has been extended through January 31, 2014. The PCIP will be replaced by marketplace coverage, but to accommodate PCIP enrollees who have not been able to obtain coverage through the marketplace, the PCIP is being extended for one month....
Read MoreHHS Announces Extensions to Enrollment and Premium Deadlines for Marketplace Coverage
The U.S. Department of Health and Human Services (HHS) recently released an Interim Final Rule that formally extends some of the marketplace (also known as the exchange) deadlines and encourages insurers to provide additional extensions if possible. Extensions Affecting the Federally-Facilitated Small Business Health Options Program (FF-SHOP) Marketplace The rule...
Read MoreNew Option for Individuals Who Have Lost Coverage to Purchase a Catastrophic Policy
Currently, catastrophic coverage only is available in the marketplace to people under age 30 and to those who do not need to meet the individual mandate either because the cost of coverage exceeds eight percent of household income or they qualify for a hardship exemption. Catastrophic plans generally will cover...
Read MoreIRS Issues Notice about Same-Sex Spouses under Section 125 Plans, Flexible Spending Accounts, and Health Savings Accounts
On Dec. 16, 2013, the Internal Revenue Service (IRS) issued Notice 2014-1 which provides some answers about covering same-sex spouses under Section 125 plans in light of the Windsor decision. In the Windsor decision, the U.S. Supreme Court ruled that the part of the Defense of Marriage Act (DOMA) that prohibited...
Read MoreDo You Understand the 2014 Requirements for Your Wellness Program?
The wellness program rules provide an exception to the general rule that employers may not take a person’s health status into account with respect to eligibility, benefits, or premiums under a group health plan. Wellness programs, therefore, are allowed if they are designed to help employees improve their health; if...
Read More7 Healthy Eating Strategies For The Holidays
Some of our most cherished traditions are centered on food, particularly at this time of year. Most dieters will tell you that December is a tough time to follow a weight-loss plan. There are sweet temptations everywhere you turn. Friends and families are getting together over festive meals. A fresh-baked...
Read MoreMaximum Deductible for 2015 – Affects Small Employers With Fully Insured Plans
HHS has announced that it expects that in 2015 the maximum deductible for insured small group plans will be $2,150 for employee-only coverage and $4,300 for family coverage (up from $2,000 and $4,000 respectively for 2014).* While there may be modifications when the final notice is released, the figures likely...
Read MoreChanges Affecting Small Insured Plans
Beginning in 2015, if an insurer agrees to use a composite rate, the rate could not be changed during the year, even if the composition of the group changes. Insurers are encouraged to follow this practice during 2014. This applies both inside and outside the SHOP marketplace. The HHS actuarial...
Read MoreTransitional Reinsurance Fee – Affects Large and Small Employers, Whether Fully Insured or Self-Funded
The Internal Revenue Service (IRS) and the Department of Health and Human Services (HHS) recently issued an update on the Transitional Reinsurance Fee (TRF) as follows: A Transitional Reinsurance Fee (TRF) will be assessed on both insured and self-funded plans for the 2014, 2015, and 2016 calendar years to help...
Read MoreOpen Enrollment for the Marketplaces – May Affect Large and Small Employers, Whether Fully Insured or Self-Funded
Open enrollment for the individual marketplaces for 2015 coverage will run from Nov. 15, 2014, through Jan. 15, 2015. Coverage would begin on Jan. 1, 2015, for individuals enrolling from Nov. 15 through Dec. 15, 2014, and on Feb. 1, 2015, for those enrolling from Dec. 16, 2014, through Jan....
Read MoreAdditional Medicare Withholding For High Earners
The Internal Revenue Service (IRS) published Final Regulations on the Additional Medicare Tax (AMT) on Nov. 29, 2013, and an updated and comprehensive FAQ on Dec. 2, 2013. There are few changes from the proposed requirements. In summary: -The requirement for additional withholding was effective Jan. 1, 2013. -The requirement applies to...
Read MoreMaximum Out-of-Pocket for 2015 – Affects Large and Small Employers, Whether Fully Insured or Self-Funded
HHS has announced that it expects that the maximum out-of-pocket limit for non-grandfathered plans in 2015 to be $6,750 for employee-only coverage and $13,500 for family coverage (up from $6,350 and $12,700 respectively for 2014). While it is possible that there will be modifications when the final notice is released,...
Read MoreMental Health Parity and Addiction Equity Act of 2008 – Key Clarifications Made By Final Regulations
The Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) seeks to ensure that medical plans, including group health plans, that provide mental health and substance use disorder benefits do so in a manner that generally is on par with the medical benefits offered under the plans. The MHPAEA...
Read MoreOur November Lunch Events Were A Huge Success!
Guests at our Fiduciary Best Practices lunch event that was held at DelFrisco’s Double Eagle Steakhouse in Philadelphia on November 14th learned more about the fee disclosure regulations that went into effect in 2011. Innovative’s own Mark Sulpizio discussed how to better understand the fee disclosures provided and address what...
Read MoreCongratulations To Dr. William F. Muhr Of South Jersey Radiology!
Innovative would like to offer heartfelt congratulations to Dr. William F. Muhr, CEO of South Jersey Radiology, on his recent recognition by the readers of South Jersey Biz magazine as one of the areas 25 most respected names in business. Readers were asked to nominate local executives who are ensuring...
Read MoreCongratulations To Bob Pekar Of Twin Oaks Community Services
Innovative would like to extend heartfelt congratulations to Bob Pekar, CEO of Twin Oaks Community Services on his recent recognition by the readers of South Jersey Biz Magazine as one of the areas 25 most respected names in business in 2013! Mr. Pekar is a licensed clinical social worker who...
Read MoreInsurers Given Permission to Renew Policies That Don’t Meet PPACA Requirements
Yesterday (Nov. 14, 2013) the White House announced that insurers will not be required to meet most of the provisions of the Patient Protection and Affordable Care Act (PPACA) if they renew individual or small group policies that were in effect on Oct. 1, 2013. The Department of Health and...
Read MoreRyan Kastner, Employee Benefits Consultant, Educates CTP Guests About PPACA
On October 24, 2013, Ryan Kastner was honored to speak to an audience of 45 about the Patient Protection and Affordable Care Act (PPACA) at a workshop conducted by Career Transition Partnership (CTP) at Temple Emanuel in Cherry Hill. Ryan walked attendees through a timeline of provisions within PPACA, focusing...
Read More2014 Cost-Of-Living Adjustments for Health Plans, Section 125 Plans and Social Security/Medicare
Many employee benefit limits are automatically adjusted each year for inflation (this is often referred to as an “indexed” limit). The Internal Revenue Service and the Social Security Administration have released the indexed figures for 2014. Because inflation is relatively low and some amounts are adjusted only if the increase...
Read MoreIRS Announces Retirement Plan Limitations For 2014
On October 31, 2013 the Internal Revenue Service and the Social Security Administration announced cost-of- living adjustments affecting dollar limitations for pension plans and other retirement–related items for the tax year 2014. The following highlights a breakdown of limits that have changed, as well as those that remain unchanged: Limits...
Read MoreAre You Ready For Thanksgiving? Tips For A Healthier Feast This Year!
Feast without Fear at Thanksgiving The average American will consume 2,500 calories or more at Thanksgiving dinner. And that doesn’t include the nibbles and drinks beforehand or the second slice of pie before bed. Check out these practical strategies for preventing heartburn after the big meal. Don’t Nibble Before Dinner...
Read MoreUBA’s Private Exchange “Benefits Passport” Is Now Open!
Employers, are you looking for an affordable insurance option to help reduce your costs, increase efficiency, simplify administration and provide exceptional value to your employees in light of Health Care Reform? Your search is over. United Benefit Advisors (UBA), the nation’s leading independent employee benefits advisory organization, announced yesterday the...
Read MoreHealth FSA “Use-It-Or-Lose-It” Rule Modified
What some would consider a long overdue change to FSA plans came down from the US Department of Treasury yesterday. The FSA “use-it-or-lose-it” provision, which has required employees to spend pre-tax dollars set aside for certain medical expenses by the end of the year or forfeit those funds, was put...
Read MoreSelf-Funded Employers Get Some Relief: Pay Only 2014 Transitional Reinsurance Fee!
Some employers with self-funded health plans can breathe a sigh of relief this week. The Department of Health and Human Services has announced that certain self-funding employers will be exempt from paying the second and third year Transitional Reinsurance Program Fees imposed by the Affordable Care Act. The first year...
Read MoreHealth Plan Benchmarking Regional Findings: How Does Your Plan Compare?
The benefits landscape remains in a state of flux as the cost of health care continues to increase and recruitment and retention of quality employees becomes more competitive. Combined with the potential impact from Health Care Reform legislation, employers are increasingly challenged to find accurate information that will help them...
Read MoreIs Eligibility For The Marketplace A Section 125 Change In Status Event For Non-Calendar Year Plans?
With the October 1st opening of the Health Insurance Marketplace, some employers have inquired about where they stand if an employee would like to leave their plan. In particular, those employers with a non-calendar year Section 125 plan have asked for guidance on whether entering the Exchange is considered a...
Read MoreBoiling Down PPACA
We’ve had a lot of employers request a simple, at-a-glance way to see all the PPACA requirements that apply to their business. This is no easy task given group size, SHOP exchanges and self-funding variables! Let’s just look at a few provisions that are effective for the plan year beginning...
Read MoreInnovative Welcomes Matt Bernstein!
We are pleased to announce the addition of Matthew Bernstein to the Innovative team. Matt is a graduate of Western New England College in Springfield, Massachusetts. As a Qualified Plan Consultant, Matt will be identifying, developing and nurturing potential client relationships in the Greater Philadelphia area. Matt is a dynamic,...
Read MoreHow Does Your Health Plan Stack Up Against Your Competitors?
See how your health plan stacks up against your competitors! Results from the United Benefit Advisors (UBA) 2013 Health Plan Survey are in! Employers can now benchmark their health plan costs and design against the nation’s largest health plan benchmarking survey of nearly 11,000 respondents. to receive a Benchmarking report...
Read MoreNew Guidance on HRAs and Premium Reimbursement Arrangements
On Sept. 13, 2013, the IRS issued Notice 2013-54, which includes details on permissible health reimbursement arrangements (HRAs), provides some clarification on minimum essential, minimum value and affordable coverage, and addresses payment of individual premiums through an employer-provided plan. HRAs Most people had expected that standalone HRAs would have difficulty...
Read MoreWhat Is A “Common Law Employee?”
As part of PPACA, every employer needs to determine whether or not they are “large” which, according to Health Care Reform, means employing 50 or more full time or full-time equivalent employees. Who exactly does this include? Contractors? While there is no set definition of a “Common Law” employee, there...
Read MoreVending Machine: Friend or Foe?
It’s not that hard to keep fruits, vegetables and other healthy snacks on hand at home. But the workplace is another story. If you haven’t brought a snack from home, you’re likely to visit the vending machine. If you look carefully, you can often find healthy – or at least...
Read MoreGOVERNMENT SHUTDOWN – NOW WHAT?
The failure of the U. S. Senate and House of Representatives to agree on a new budget for the Fiscal Year (beginning October 1) is resulting in a furlough of more than 800,000 federal workers and government agencies temporarily closing or cutting back the operations of numerous federal facilities and...
Read MoreIRS Provides Process to Correct Over-Withholding of Same-Sex Spouse Benefits
On Sept. 23, 2013, the IRS issued Notice 2013-61. This notice provides a special process for employers to make refund claims or internal adjustments of FICA and federal income tax (FIT) that was withheld or paid in connection with same-sex spouse benefits. Employers that prefer to use the normal refund...
Read MoreHighlights of the SHOP Exchange
PPACA requires that a Small Business Health Options Program (SHOP) exchange/marketplace be established in each state for small employers. For 2014, all states will use 50 employees as the cut-off for small employer status.* Beginning in 2016, all states must use 100 employees as the cut-off. The SHOP exchanges/marketplaces will...
Read MoreDOL Announces Non-Enforcement of Marketplace/Exchange Notice
PPACA requires employers covered by the Fair Labor Standards Act to provide a notice about the upcoming health marketplaces (also called exchanges) to their employees. The notice is due Oct. 1, 2013. On Sept. 11, 2013 the Department of Labor (DOL) announced that it will not penalize employers that do...
Read MoreA Delay for Out-Of-Pocket Maximums
A few weeks ago several media outlets picked up a FAQ that the Department of Labor issued in February of this year. The FAQ may be accessed here: FAQs About Affordable Care Act Implementation Part XII Some of the reports have created confusion about the requirement, and the scope of...
Read MorePractice Positivity to Help Beat Stress
Being a positive thinker can affect your life more than you realize. Practicing positive thinking may make you a healthier person. Lower rates of heart disease and mental illness are linked to positive thinking. Positive psychology is a new branch of psychology that’s about 15 years old. Specialists in positive...
Read MoreIRS Releases Proposed PPACA Reporting Rules
On Sept. 5, 2013, the Internal Revenue Service (IRS) released the long-awaited rules that describe the reporting that plans, employers, and insurers will need to provide in support of the individual shared-responsibility and employer shared-responsibility requirements of the Patient Protection and Affordable Care Act (PPACA). The rules are proposed, so...
Read MoreHighlights of Exchange Notice Requirement
Most employers must give a notice about the upcoming health exchanges/marketplaces to all existing employees by Oct. 1, 2013. Employees hired after that date must receive the notice within 14 days following their start date. All employers who are subject to the Fair Labor Standards Act must give the notice....
Read MoreFrequently Asked Questions about the Exchange (Marketplace) Notice
This FAQ is based on Department of Labor (DOL) Technical Release 2013-02, which does not provide specific guidance on many issues. Consequently, some of the answers in this FAQ are based on agency guidance provided in similar situations. The answers in this FAQ assume the employer is completing the model...
Read MoreIRS Issues Rules on Same-Sex Marriages
On Aug. 29, 2013, the IRS issued Revenue Ruling 2013-17, which describes how the IRS will handle same-sex marriages for federal tax purposes in light of the U.S. Supreme Court decision that found a part of the Defense of Marriage Act (DOMA) unconstitutional. The ruling says: The IRS will consider...
Read MoreThe October 1st Deadline Is Just Around The Corner: Employers Must Provide Notices Regarding Availability of Exchange Coverage
A provision of the 2010 health care reform law requires employers to provide notices to all employees regarding the availability of health coverage options through the state-based exchanges created pursuant to that law. The DOL issued temporary guidance on May 8, 2013 (Technical Release 2013-02) and model notices for employers...
Read MoreEnsure Employee Health and Reap the Benefits
It sounds simple enough: improve workforce health, reduce health care costs. It’s a private matter, one’s health, but many employers invest in on-site exercise equipment, sports teams or any number of activities that not only promote camaraderie, but wellness as well. On the other side of the coin, many more...
Read MoreThe Real Story on Out-Of-Pocket Maximums
Last week several media outlets picked up a FAQ that the Department of Labor issued in February of this year. The FAQ may be accessed here: FAQs about Affordable Care Act Implementation Part XII Some of the reports have created confusion about the requirement, and the scope of what has...
Read MoreFrequently Asked Questions About Grandfathered Plans – Part Two
Those employers with grandfathered status need to decide if maintaining grandfathered status is their best option for the coming year. Here is a continuation of the questions asked most frequently, and answers, about grandfathering a group health plan. Q5: How are changes measured? A5: Changes are measured cumulatively since March...
Read MoreFrequently Asked Questions About Grandfathered Plans – Part One
As employers determine their plan designs for the coming year, those with grandfathered status need to decide if maintaining grandfathered status is their best option. Following are some frequently asked questions, and answers, about grandfathering a group health plan. Q1: May plans maintain grandfathered status after 2014? A1: Yes, they...
Read MoreSeafood, Your Healthy Heart Hero
Seafood and Your Healthy Heart Following a healthy diet is a proven way to reduce your risk of heart disease. Pairing healthy eating with a physically active lifestyle will lower that risk even more. Most of us know which types of food can contribute to heart disease. We try to...
Read MoreThe Individual Mandate: Noteworthy Numbers
For 2013: The tax filing threshold is $10,000 if filing single and $20,000 if married and filing jointly. Federal Poverty Level (FPL) in the 48 contiguous states is $11,490 for a single household and $45,960 for household of four. It is $14,350/29,440 in Alaska and $13,230/27,090 in Hawaii. The subsidy...
Read MoreIndividual Mandate: Who Is Exempt?
While most people must obtain coverage or pay penalties, individuals in these situations will not be penalized if they do not obtain coverage: They do not have access to affordable coverage (cost exceeds 8 percent of modified adjusted gross household income) Their household income is below the tax filing...
Read MoreIndividual Mandate: Who Is Eligible For Premium Subsidies?
To help lower-income people meet the requirement to have insurance, a premium subsidy will be available to a person who: Purchases coverage through a public marketplace/exchange; and Has a household modified adjusted gross income between 100 or 133 percent (depending on their state) and 400 percent of Federal Poverty Level...
Read MorePPACA And The Individual Shared Responsibility Requirement
Although the employer shared responsibility requirements have been delayed to 2015, the individual responsibility requirement (also known as the individual mandate) is still scheduled to take effect in 2014. Under the individual mandate, most people residing in the U.S. will be required to have minimum essential coverage, or they will...
Read MoreMLR REBATE CONSIDERATIONS – PRIVATE PLANS
As was the case last year, insurers with medical loss ratios (MLRs) that were below the prescribed levels on their blocks of business must issue rebates to policyholders. Insurers must pay rebates owed on calendar year 2012 experience by Aug. 1, 2013. The rules for calculating and distributing these rebates...
Read MoreMLR REBATE CONSIDERATIONS – GOVERNMENT AND CHURCH PLANS
As was the case last year, insurers with medical loss ratios (MLRs) that were below the prescribed levels on their blocks of business must issue rebates to policyholders. Insurers must pay rebates owed on calendar year 2012 experience by Aug. 1, 2013. The rules for calculating and distributing these rebates...
Read MoreIRS Confirms Play or Pay Delay
On July 9, 2013 the Internal Revenue Service issued Notice 2013-45, which confirms that the employer shared responsibility penalties and reporting requirements will not apply until 2015. Last week the Department of the Treasury and the White House blogged that this announcement was coming. The IRS Notice states that employers...
Read MorePlay It Safe Outside!
BUGS BEWARE! Mosquitoes, ticks and people all share the great outdoors as their playground. The insects may be more than a nuisance to be swatted away. In the U.S., mosquitoes may transmit some rare but serious diseases including West Nile virus, St. Louis encephalitis, dengue and eastern equine encephalitis. Ticks...
Read MoreSpanish Version of Notice of Exchange is Now Available
The DOL has provided Spanish versions of the model notice regarding the exchange/health insurance marketplace. While employers are not specifically required to provide the Spanish version to Spanish-speaking employees, since the notice is supposed to be understandable by the average employee, providing the Spanish version where appropriate is advisable. There...
Read MorePlay or Pay Penalty Delayed To 2015
On July 2, 2013 the Department of the Treasury and the White House used their blogs to announce that the employer reporting requirements, and the employer shared responsibility/Play or Pay penalty, are being delayed until 2015. The Treasury said that it will provide a formal announcement and additional details next...
Read MorePPACA: Individual Grace Period
Effective Date for Individual Mandate Delayed For Some People On June 26, 2013 the IRS unexpectedly issued a notice that gives individuals who are eligible for coverage under an employer-sponsored health plan, but who have not elected coverage under that plan, until the start of the 2014 plan year to...
Read MoreU.S. Supreme Court Rules Legally-Married Same-Sex Spouses Entitled to Federal Recognition and Lifts California Ban on Same-Sex Marriage
The United States Supreme Court has issued two decisions that expand same-sex marriage rights. In the first, United States v. Windsor, No. 12-307 (June 26, 2013), the Court ruled unconstitutional a law denying federal recognition of legally-married same-sex couples. In the second, Hollingsworth, et al. v. Perry, No. 12-144 (June...
Read MoreThe 2013 UBA Health Plan Benchmarking Survey Has Closed And The Winner Of The iPad Is…
THE WINNER IS: The Philadelphia Zoo!!! We had an overwhelming response to our 2013 UBA Health Plan Benchmarking Survey and we are happy to announce that we have randomly picked the winner for the Apple 32 GB iPad! With over 18,000 plans participating, including more than 75 plans from our...
Read MoreHave You Made Any “Material Modifications” To Your Plan Since Your Last SBC Was Issued?
If a group health plan or health insurance issuer have made any material modification (during the plan year) in terms of the plan or coverage involved that’s not reflected in the most recent Summary of Benefits and Coverage (SBC), the plan or issuer must provide notice of the modification to...
Read MoreCOMPLIANCE ALERT!! Final “SHOP” Regulations Issued
On June 4, 2013, the Department of Health and Human Services (“HHS”), Centers for Medicare & Medicaid Services (“CMS”), issued final regulations implementing the provisions of the Affordable Care Act (“ACA”) related to the establishment and operation of the Small Business Health Options Program (“SHOP”). The final regulations delay by...
Read MorePCORI Fee Due Date
By July 31, 2013, most issuers of health insurance policies and plan sponsors of self-insured health plans must pay a fee of $1 per covered life as a result of new provisions in the Patient Protection and Affordable Care Act. The fee will partially fund the Patient-Centered Outcome Research Institute...
Read MorePPACA: Certificates of Creditable Coverage
Affects all plans, whether fully insured, self-funded or grandfathered, and regardless of employer size, as of Jan. 1, 2015. Because pre-existing condition limitations will not be permitted after the start of the 2014 plan year, certificates of creditable coverage would not need to be provided after Dec. 31, 2014. (This...
Read More8 Men’s Health Myths Exposed
Men get their health news from many sources: friends at the gym, their doctors, current publications and the Internet. A lot of the information is accurate. Some of the info mixes truth and rumor. Some of it is just plain wrong. Let’s take a look at eight popular myths about...
Read MoreAGENCIES ISSUE FINAL RULES ON WELLNESS PROGRAMS
On May 29, 2013 the Department of Health and Human Services, the Internal Revenue Service and the Department of Labor jointly issued a final rule that addresses how wellness programs must operate under PPACA beginning in 2014. In many respects the final rules carry forward the rules that have been...
Read MoreHealth Care Reform Lunch Events Scheduled for July – Register Now!
In the last few weeks, Innovative hosted two more Health Care Reform seminar lunch events in Weehawken and Marlton. Since the November election we have hosted ten of these events, and have been requested to present at several networking events. The feedback on our program is excellent and we appreciate...
Read MoreDo You Know What The Summary Of Benefits & Coverage Requirements Are Under Health Care Reform?
A Summary of Benefits & Coverage (SBC) is required starting the first day of the first plan year after September 23, 2012, or the first day of the first open enrollment period after this date. Health insurers and group health plans must provide the SBC and the Uniform Glossary to...
Read MoreCOMPLIANCE ALERT! Employers Must Provide Notices Regarding Availability of Exchange Coverage
A provision of the 2010 health care reform law requires employers to provide notices, by March 1, 2013, to all employees regarding the availability of health coverage options through the state-based exchanges created pursuant to that law. In January, the Department of Labor had announced delayed enforcement of the exchange...
Read MoreA Great Day at the Tri-State SHRM Expo!
As both an exhibitor and speaker at the May 13th event in Mount Laurel, we had a great time meeting and speaking with all of the attendees. Our custom-made fortune cookies were a big hit! Terriann spoke at a breakout session on the topic of Play or Pay within PPACA. ...
Read MoreWomen’s Health Myths
Do you go online to learn about your health? You’re not alone. A recent Pew survey showed 72% of Internet users looked for health info online. And women are more likely to do so than men. But you do need to be careful. Not all health sites are accurate. And...
Read MoreAN UPDATED SUMMARY OF BENEFITS AND COVERAGE FORM AND ANNUAL LIMITS WAIVERS
The agencies have released an updated Summary of Benefits and Coverage (SBC) template that plans will need to use for 2014. The updated template has very few changes from the version used for 2013. The primary change is that the 2014 SBC must state whether or not the plan provides...
Read MoreWellness Incentives and the Play or Pay Requirement
The Departments of Labor, Health and Human Services and the Treasury have issued several updates that affect employer-sponsored group health plans. Wellness Incentives, HRAs, Minimum Value and Affordability The IRS has released proposed regulations that address how wellness incentives or penalties are applied to premium affordability (for purposes of the...
Read MoreThe Department of Labor Begins Auditing Group Health Plans for PPACA, GINA and Wellness Program Compliance
Employers that have had their group health plans audited by the Employee Benefits Security Administration (EBSA, the arm of the U.S. Department of Labor that enforces Title I of ERISA) are aware of the broad nature of the document requests and compliance reviews carried out under these audits. The EBSA...
Read MoreInnovative Welcomes Stayce Godfrey-Smith To Our Team!
Stayce joined the Innovative team mid-April as a Benefits & Eligibility Specialist. Her extensive background in health and welfare administration will prove invaluable in her new role, as will her experience in client service and management. As an integral addition to our Account Management team, we are confident that Stayce...
Read MoreCOMPLIANCE ALERT! Important Transition Relief for Non-Calendar Year Plans
The January 1, 2014 effective date of the Pay-or-Play requirements under health care reform presents special issues for employers with non-calendar year plans. Prior to the release of the proposed regulations under the shared responsibility rules, employers with non-calendar year plans would either need to comply with the Pay-or-Play requirements...
Read MoreInnovative Is Proud To Support the Seventh Annual American Heart Association Go Red for Women Luncheon!
On Thursday April 11, 2013 Innovative attended the Go Red for Women Lunch Event at Lucien’s Manor in Berlin, New Jersey. Today, heart disease is STILL the #1 killer of women, causing 1 in 3 deaths each year. But it can be prevented. Knowledge of the risk factors for heart...
Read MoreEssential Health Benefits, Minimum Essential Coverage, Minimum Value Coverage – What’s The Difference?
The Patient Protection and Affordable Care Act (PPACA) uses terms that sound alike for three very different things. Here’s a closer look at these terms, and when they’re used. Essential Health Benefits Significantly affects individuals and small employers with a fully insured plan. Has a limited impact on self-funded and...
Read MoreManaging Seasonal Allergies
The Worst Offenders Seasonal allergy is caused by tree pollen in the early spring. During the late spring and early summer, the irritating pollen is usually from grasses. Weeds are the typical pollen source in late summer and into the fall. Tree Pollen In springtime, trees release huge amounts of...
Read MoreEmployers, Do You Know What You Need To Do Before January 2014 To Comply With PPACA?
The provisions associated with health care reform pose many questions for employers, most importantly, what do I need to do and when? Here is a checklist of items to cross off your list before January 2014: Calculate and pay the Patient Centered Outcome Fee if the plan is self-funded (insurers...
Read MoreREGISTER NOW!! Health Care Reform Lunch ‘N Learn Events in Weehawken and Marlton
Since the November Presidential election, Innovative has hosted eight Lunch N’ Learn events in New Jersey, Pennsylvania and New York, and we have just added two more! We will be having our first Weehawken event at The Chart House Restaurant this month on April 24th, and we will be back...
Read MorePPACA Update: External Claims Appeals Requirement
Applies to all nongrandfathered plans, whether fully insured or self-funded, and to all sizes of employers. PPACA requires all nongrandfathered plans to follow detailed processes for claims appeals, including a process for external review that includes 16 consumer protections required under the NAIC model act. Due to practical difficulties meeting...
Read MoreTerriann to Speak about Health Care Reform at Tri-State HRMA’s 27th Annual Conference
Since the election in November, Terriann Procida has been educating employers about Health Care Reform, specifically the new Play or Pay regulation. Do you know what you need to do to begin budgeting for the 2013-2014 PPACA Provisions? Do you understand how potential penalties associated with Play or Pay may...
Read MorePPACA Update: Certificates of Creditable Coverage
Affects all plans, whether fully insured, self-funded or grandfathered, and regardless of employer size, as of Jan. 1, 2015. Because pre-existing condition limitations will not be permitted after the start of the 2014 plan year, certificates of creditable coverage would not need to be provided after Dec. 31, 2014. (This...
Read MorePPACA Update: Eligibility Waiting Periods
Affects all plans, whether fully insured, self-funded or grandfathered. Applies to all sizes of employers, as of the start of the 2014 plan year. The agencies have issued proposed regulations that state that an eligibility waiting period cannot be more than 90 days. This literally is 90 calendar days —...
Read MorePPACA Employer Fees: Patient-Centered Outcomes Research Institute (PCORI) and Transitional Reinsurance (TRF)
The IRS and the Department of Health and Human Services have issued final regulations that provide details on two new, temporary fees that will be due as part of the Patient Protection and Affordable Care Act (PPACA). These fees will be calculated and paid directly by self-funded plans. The fees...
Read MorePlay or Pay: Non-Calendar Year Transition Rules for Measuring in 2013
A non-calendar year plan that had coverage in place on Dec. 27, 2012: Will not owe the “inadequate coverage penalty” on any employee who was eligible for coverage on Dec. 27, 2012 (and on employees hired after that date, if they would have been eligible under the rules in effect...
Read MoreInnovative Attends Saint Joseph’s University Career Fair
Innovative Benefit Planning is looking for highly motivated individuals to join our growing team. As a part of our recruiting initiative, we participated in the spring 2013 Career Fair at Saint Joseph’s University where we were among 161 companies searching for the best and the brightest. The turnout was impressive,...
Read MoreFinal Regulations Issued on Market Reforms-Fair Health Insurance Premiums for Fully Insured Health Care Plans
Impacts all non-grandfathered fully insured small group plans (both in and outside the exchange) beginning with the 2014 plan year: The changes in the rules that apply to fully insured small groups, whether the coverage is provided inside or outside the exchange, are significant. From an employer standpoint, the most...
Read MoreFinal Regulations Issued on Market Reforms-Guaranteed Access for Fully Insured Health Care Plans
Impacts all nongrandfathered fully insured plans, whether inside or outside the exchange, beginning with the 2014 plan year: Guaranteed issue and renewal will apply to all insured plans regardless of size. Participation and employer contribution requirements will not be permitted under the guaranteed availability rules, although insurers may impose participation...
Read MoreFinal Regulations Issued on Essential Benefits and Actuarial Value for Fully Insured Health Care Plans
Impacts non-grandfathered small-group plans (both in and outside the exchange) beginning with the 2014 plan year: Beginning with the 2014 plan year all nongrandfathered plans in the small group market – whether inside or outside the exchange – will need to provide the “essential health benefits package” (EHB package). The...
Read MoreIt’s Time to Get Your Yoga On!
Yoga and Back Pain Prevention Lack of exercise is a risk factor for developing back pain. Exercise not only strengthens the muscles of the back, neck and shoulders, but it also relaxes the back, reduces pain and increases flexibility. It is recommended to do 15 to 30 minutes of back...
Read MoreFAQ Released: Final Regulations Issued on Minimum Value for Self-Funded Health Care Plans
Impacts all self-funded plans as of the start of the 2014 plan year Self-funded plans (regardless of size) will not be required to provide the ten “essential health benefits” or coverage at a “metal level” as some plans will be required to do. (The essential health benefits are coverage within...
Read MoreFAQ Released: Final Regulations Issued on Minimum Value for Fully Insured Health Care Plans
Impacts large fully insured plans with 50 or more employees: Large group insured plans are not required to provide the ten “essential health benefits” or coverage at a “metal level” as small plans will be required to do. (The essential health benefits are coverage within these categories – ambulatory/outpatient, emergency,...
Read MoreCOMPLIANCE ALERT: Labor Department Releases New FMLA Model Forms and Notice Poster
The U.S. Department of Labor has released revised model Family and Medical Leave Act (“FMLA”) forms to administer federal FMLA leave and a notice poster. The updated forms should be used by employers immediately, although they include no substantive revisions despite recent rulemaking on the FMLA military caregiver leave provisions...
Read MoreSelf-Funded Health Care Plans FAQ Released: Final Regulations Issued on Out-of-Pocket Limits
Impacts all non-grandfathered self-funded plans beginning with the 2014 plan year The FAQ also talks about the out-of-pocket maximum requirements. Beginning with the 2014 plan year, plans may not have an out-of-pocket maximum that is larger than the allowed out-of-pocket limit for high-deductible health plans (HDHP) issued in connection with...
Read MoreFully Insured Health Care Plans FAQ Released: Final Regulations Issued on Out-of-Pocket Limits
Impacts all nongrandfathered fully insured plans beginning with the 2014 plan year: The FAQ also talks about the out-of-pocket maximum requirements. Beginning with the 2014 plan year, plans may not have an out-of-pocket maximum that is larger than the allowed out-of-pocket limit for high-deductible health plans (HDHP) issued in connection...
Read MoreCOMPLIANCE ALERT: Labor Department Releases New FMLA Model Forms and Notice Poster
The U.S. Department of Labor has released revised model Family and Medical Leave Act (“FMLA”) forms to administer federal FMLA leave and a notice poster. The updated forms should be used by employers immediately, although they include no substantive revisions despite recent rulemaking on the FMLA military caregiver leave provisions...
Read MoreSelf-Funded Health Care Plans FAQ Released: Final Regulations Issued on Preventive Care
Impacts all non-grandfathered, self-funded plans now: The agencies have received many questions about the requirement to provide first-dollar preventive care. They have now issued a FAQ that clarifies that: While plans generally do not need to provide out-of-network preventive care if there are no in-network providers able to provide the...
Read MoreFully Insured Health Care Plans FAQ Released: Final Regulations Issued on Preventive Care
Impacts all non-grandfathered fully insured plans now: The agencies have received many questions about the requirement to provide first-dollar preventive care. They have now issued a FAQ that clarifies that: While plans generally do not need to provide out-of-network preventive care if there are no in-network providers able to provide...
Read MoreFAQ Released: Final Regulations Issued on Whistleblowing for Self-Funded Health Care Plans
Impacts all self-funded plans beginning April 2013 PPACA prohibits employers (including insurers) from retaliating against an employee for reporting possible violations of PPACA to his employer or to the government, providing testimony about the possible violation or refusing to violate the law. It also prohibits retaliating or taking an unfavorable...
Read MoreFAQ Released: Final Regulations Issued on Whistleblowing for Fully Insured Health Care Plans
Impacts all fully insured plans beginning April 2013 PPACA prohibits employers (including insurers) from retaliating against an employee for reporting possible violations of PPACA to his employer or to the government, providing testimony about the possible violation or refusing to violate the law. It also prohibits retaliating or taking an...
Read MoreThe “Set Sail: Samaritan Celebration of Life Gala” Was A Great Success Once Again!
The Samaritan Healthcare & Hospice Annual Gala took place Saturday February 23rd with a “Cruise” theme, complete with music, dancing, gambling, auction, and of course, great food! Kathy Orr, CBS 3 Eyewitness News Emmy-Award-Winning Meteorologist brought great energy to the event as the emcee. With over 230 in attendance, the...
Read MoreTerriann Scheduled to Speak about Health Care Reform at Tri-State HRMA’s 27th Annual Conference
Since the election in November, Terriann Procida has been educating employers about Health Care Reform, specifically the new Play or Pay regulation. Do you know what you need to do to begin budgeting for the 2013-2014 PPACA Provisions? Do you understand how potential penalties associated with Play or Pay may...
Read MoreDo You Monitor Your 3(38) Adviser?
If you don’t, maybe you should. Many people mistakenly assume that when they hire a 3(38) they no longer have to worry about any fiduciary responsibility. They are wrong. While they wouldn’t necessarily be held responsible for the day-to-day decisions made by the 3(38), over time, if they are not...
Read MorePPACA’s “Affordability” Requirement is Clarified by the IRS
The IRS finalized a rule that clarified that the health coverage “affordability” requirement (that an employee’s premium contribution not exceed 9.5 percent of household income) under the Patient Protection and Affordable Care Act (PPACA) will be based on self-only coverage, according to a Business Insurance online report. Employers with plans...
Read MorePPACA Update: Women’s Preventive Services
Proposed rules that would make it simpler for religious organizations and religious-affiliated not-for-profit organizations like hospitals and schools that have a religious objection to providing contraceptive services were released by the DOL on Feb. 1, 2013. These employers would notify their insurer of their objection, and the insurer automatically would...
Read MoreInnovative Benefit Planning Welcomes Ryan Kastner to the Team!
We are pleased to announce the addition of Ryan Kastner to the Innovative team. Ryan is a graduate from the Perdue School of Business at Salisbury University in Maryland. As an Employee Benefits Consultant, Ryan will be identifying, developing and nurturing potential client relationships in the Greater Philadelphia area. Earning...
Read MorePPACA Update: Minimum Essential Coverage
On Feb. 1, 2013, HHS and the IRS issued two proposed regulations that provide details on the individual shared responsibility requirement. PPACA requires that non-exempt individuals obtain “minimum essential coverage” or pay a penalty. Minimum essential coverage includes individual insurance, Medicare, Medicaid, CHIP, TRICARE, VA and similar government programs, and...
Read MorePPACA Update: IRS Issues Final Regulation on Tax Credits
On Feb. 1, 2013, the IRS issued a final regulation that provides the long awaited answer of whether family members of an employee who has access to affordable self-only coverage are eligible for a premium tax credit/subsidy. The answer is that they are not – if the employee has access...
Read MoreHRA Restrictions Under PPACA
Because PPACA prohibits annual dollar limits on essential health benefits, HRAs that are not integrated with other group health coverage (usually a major medical plan) will not be permitted after Jan. 1, 2014. The January 24, 2013 DOL FAQ states that an employer-provided HRA will not be considered integrated (and...
Read MorePPACA Update: Notice of Exchange Has Been Delayed
The Department of Health and Human Services (HHS), the Internal Revenue Service (IRS) and the Department of Labor (DOL) have recently issued more FAQs and proposed rules that address several employer obligations under the Patient Protection and Affordable Care Act (PPACA). On Jan. 24, 2013, the DOL issued a FAQ...
Read MoreAre You Trying To Stick With A Healthier Eating Plan? If So, What Should You Do When You Go Out To Eat?
Restaurant Strategies When Dining Out Keep this baker’s dozen of tips in mind next time you eat out to help you prevent mindless overeating: Avoid all-you-can-eat restaurants, especially if you’re likely to try to “get your money’s worth” with the sheer quantity of food. This style of dining is no...
Read MoreCOMPLIANCE ALERT! Final HIPAA Privacy Regulations are Published
The Office for Civil Rights (“OCR”) of the U.S. Department of Health and Human Services published its long-awaited final privacy and security regulations (“Final Rule”) under the Health Insurance Portability and Accountability Act (“HIPAA”) on January 25, 2013. The Final Rule becomes effective March 26, 2013, and, in general, covered...
Read MoreInnovative Supports the Samaritan Healthcare & Hospice Gala!
For the third consecutive year Terriann Procida is Chairing the Samaritan fundraising gala. This year the theme is “Set Sail: Samaritan Celebration of Life Gala” and it will take place on Saturday, February 23, 2013 at The Westin Mount Laurel. Samaritan has provided hospice care for more than 55,000 families...
Read MoreWhat All Employers Need to Know About the “Cadillac Tax”
Starting in 2018, employers offering health plans that exceed a certain cost (the total employee and employer cost) would be subject to a 40% excise tax on the amount above that value. For individual coverage, the threshold would be $10,200 and for family coverage the threshold would be $27,500.* The...
Read MoreCoordinating Exchange and Plan Open Enrollments
On Jan. 2, 2013, the IRS issued a detailed rule that, among other things, provides that noncalendar-year plans may amend their Section 125 plans to allow employees to make midyear changes because of PPACA. Open enrollment for the exchanges will begin in October 2013 for a Jan. 1, 2014, effective...
Read MoreHow Will an Employer Know if an Employee Applies for a Premium Subsidy in the Exchange?
On Jan. 14, 2013, the Department of Health and Human Services (HHS) issued another lengthy proposed rule under the Patient Protection and Affordable Care Act (PPACA). Among other things, the proposed rule provides some information on how employers will be notified if an employee applies for a premium subsidy /...
Read MoreTerriann Presents to the Philadelphia Chapter of Women Presidents’ Organization!
As an area business owner herself, and an expert on Health Care Reform, Terriann Procida is honored to present “Health Care Reform: An Update on PPACA Since the Election” to the Philadelphia Chapter of Women Presidents’ Organization. The PPACA provisions present some challenges to employers in deciphering the new regulations...
Read MorePPACA: What Do Employers Need To Do Between Now And January 2014?
The provisions associated with health care reform pose many questions for employers, most importantly, what do I need to do and when? Here is a checklist of items to cross off your list before January 2014: Calculate and pay the Patient Centered Outcome Fee if the plan is self-funded (insurers...
Read MoreStand, Stretch and Move!
A Vanderbilt University study estimated that Americans spend about 55 percent of waking time sitting. That’s about seven and a half hours in a chair every day. A growing body of research shows that long periods of physical inactivity raise your risk of developing heart disease, Type 2 diabetes, cancer,...
Read MoreWhat Should Employers Already Be Doing To Comply With PPACA?
Plans: May not have a lifetime dollar maximum on any “essential health benefit” May not have an annual dollar limit on an “essential health benefit” that is over a certain amount Must cover the employee’s dependent children until the dependent reaches age 26 – even if the child...
Read MoreThanks to the Fiscal Cliff Deal, Roth 401(k) Conversions Are Allowed for All
As part of the fiscal cliff deal employees have been given the ability to take funds in a pre-tax 401(k) account and convert it into a Roth 401(k) account. Prior to this most recent provision in the American Taxpayer Relief Act of 2012, only amounts that were deemed distributable could...
Read MoreHealth Care Reform Update: IRS Proposes Regulations on Employer Penalty
The Internal Revenue Service has released proposed regulations on the health care reform employer “shared responsibility” penalty provision. This is the penalty on “large” employers (those with at least 50 full-time or full-time equivalent employees) that do not provide affordable minimum essential coverage for full-time employees and their dependents and...
Read MoreCompliance Alert! DOL Begins Auditing Group Health Plans for PPACA, GINA and Wellness Program Compliance
Employers that have had their group health plans audited by the Employee Benefits Security Administration (EBSA, the arm of the U.S. Department of Labor that enforces Title I of ERISA) are aware of the broad nature of the document requests and compliance reviews carried out under these audits. The EBSA...
Read MoreIndividual Mandate Tax – What is the Cost for Non-Compliance?
Last June the Supreme Court ruled that PPACA, including the individual mandate, is constitutional. Under the law, individuals are required to purchase health care insurance and if they do not, the penalty will be a tax. In order to avoid this tax, a person must have “minimum essential” coverage. This...
Read MoreHHS ISSUES PROPOSED RULES ON ‘BENEFIT AND PAYMENT PARAMETERS,’ MULTI-STATE PLAN PROGRAM
The following is a summary of proposed regulations. Some or all of the provisions may change when final rules are issued. On Dec. 5 and 7, 2012, the Department of Health and Human Services (HHS) issued two more sets of proposed rules that provide added details on how the Patient...
Read MoreHealth Care Reform Lunch N’Learns a Huge Success! More to come…
In light of the outcome of the November Presidential election, Innovative hosted three Lunch N’ Learn events over the last few weeks at Fleming’s Steak House in Marlton, DelFrisco’s Steak House in Philadelphia and Ruth’s Chris Steak House in Parsippany. We also joined Ultimate Software at a fourth event at...
Read MoreMake Time – and Space – for Workouts
Create a Home Gym Cold weather and short days make it harder to exercise outdoors in the winter. For those times when it’s too wet, too cold or just too dark to work out outdoors, why not retreat to your own home gym? For a minimal investment, you can transform...
Read MoreHIGHLIGHTS OF PROPOSED RULES ON HEALTH INSURANCE MARKET RULES
On Nov. 20, 2012, the Department of Health and Human Services (HHS) issued proposed rules that address a number of health insurance market reforms. The rule is still in the “proposed” stage, which means that there may — and likely will — be changes when the final rule is issued....
Read MoreHIGHLIGHTS OF PROPOSED RULES ON WELLNESS PROGRAMS
On Nov. 20, 2012, the Department of Health and Human Services, the IRS and the Department of Labor jointly issued a proposed rule that addresses how wellness programs may operate under PPACA beginning in 2014. The proposed rule would largely carry forward the rules that have been in effect for...
Read MoreHIGHLIGHTS OF PROPOSED RULES ON ESSENTIAL HEALTH BENEFITS AND ACTUARIAL VALUE
On Nov. 20, 2012, the Department of Health and Human Services (HHS) issued a proposed rule that addresses a number of questions surrounding essential health benefits and determining actuarial and minimum value. This rule is still in the “proposed” stage, which means that there may — and likely will —...
Read MoreCORRECTING OPERATIONAL MISTAKES CAN ELIMINATE FIDUCIARY LIABILITY
Over the past decade, plan sponsors have become familiar with the voluntary correction programs offered by the IRS and Department of Labor, including the Service’s Employee Plans Compliance Resolution System (EPCRS) and the DOL’s Voluntary Fiduciary Correction Program (VFCP). These programs offer formal ways for sponsors to correct certain administrative...
Read MoreHealthy Employees Lead to Wealthy Employees
We all know that employer-sponsored wellness programs are effective at extending quality of life by maintaining good health and reducing health risks that can worsen over time. Companies also obtain financials savings from implementing wellness programs. For instance, for every dollar spent on wellness, medical costs are reduced by $3.27...
Read MoreInnovative Welcomes Michelle Bross!
We are so excited to welcome Michelle Bross to the Innovative team! Michelle comes highly recommended and her extensive background in office administration will be well utilized as Innovative continues to grow. Best of luck in your new role Michelle!
Read MoreCritical Amendment Deadline Approaching for Defined Benefit Plans
Sponsors of single-employer defined benefit pension plans will need to amend those plans soon to comply with a critical requirement of the Pension Protection Act of 2006 (the PPA). As explained more fully below, meeting this deadline is crucial because the IRS has conditioned anti-cutback relief on a timely amendment. ...
Read MoreHealth Plan Design Drives Regional Costs
United Benefit Advisors (UBA), one of the nation’s largest employee benefit advisory organizations, announces more key findings from its 2012 Health Plan Survey. As health care costs continue to increase and recruitment and retention of quality employees becomes more competitive, accurate and detailed benefits benchmarking data is imperative for employee...
Read MoreWhat Employers Need To Know Right Now About Health Care Reform And What The Election Results Mean For PPACA
Maintenance of the status quo in Washington, D.C. (the re-election of Barack Obama, with a Republican majority in the House of Representatives and a Democratic majority in the Senate) means that implementation of the Patient Protection and Affordable Care Act (PPACA) will move forward largely as the law was passed...
Read MoreIn this Election, Health Care Takes Center Stage
By Thomas Mangan, CEO, United Benefit Advisors UBA and CFO magazine weigh in on the health insurance exchange market in the face of health care reform. Today marks a historic milestone in the leadership of America as millions of people head to the polls to elect or re-elect our president....
Read MoreThe Benefits of Napping
Quick Takes Naptime – Not Just for Toddlers Lions nap, dogs nap, even dolphins take brief naps. In fact, 85% of all mammal species are polyphasic sleepers, meaning that they sleep for short periods throughout the day. Generally, humans are monophasic sleepers, meaning we divide the day into two parts,...
Read MorePlay or Pay: Applying the Employer Shared Responsibility Penalties
PPACA calls for two possible penalties, one for not offering “minimum essential” coverage and a different penalty for offering coverage that is considered inadequate because it is not “affordable” and/or it does not provide “minimum value.” (A) The “no offer” penalty applies if the large employer does not offer “minimum...
Read MorePlay or Pay: How Does an Employer Determine Average Hours Worked?
An employer may simply look at its population on a current, month by month basis if it wishes to. However, to avoid the complications that may arise if an employee alternates between working more and less than 30 hours, or to simply reduce calculation frequency, IRS Notice 2012-58 gives an...
Read MoreCOMPLIANCE ALERT: 2013 Annual Benefit Plan Amounts
2013 INFLATION ADJUSTMENTS Following recent announcements by both the IRS and the Social Security Administration, we now know most of the dollar amounts that employers will need to administer their benefit plans for 2013. Many of the new numbers are slightly higher than their 2012 counterparts. For instance, the annual...
Read MorePlay or Pay: How Will An Employer Count Hours?
It is expected that current DOL rules for counting hours for pension plan purposes will be used to count an employee’s hours of service as a full-time employee or full-time employee equivalent. Under these rules, a person is considered to have completed an “hour of service” with each hour for...
Read MoreCOMPLIANCE ALERT! CRITICAL AMENDMENT DEADLINE APPROACHING FOR DEFINED BENEFIT PLANS
Sponsors of single-employer defined benefit pension plans will need to amend those plans soon to comply with a critical requirement of the Pension Protection Act of 2006 (the PPA). As explained more fully below, meeting this deadline is crucial because the IRS has conditioned anti-cutback relief on a timely amendment. ...
Read MoreThe Play or Pay Penalty – How Are Employees Counted Under PPACA?
Determining how many employees you have is important for several purposes under the Patient Protection and Affordable Care Act (PPACA). So far, no final rules have been issued, but on Aug. 31, 2012, the regulatory agencies issued safe harbors for 2014 on several key issues. The agencies have also provided...
Read MoreImportant Information About New Jersey 51-100 Health Benefits Plans
A benefit feature that encourages use of generic drugs will be included in all 51-100 health benefits plans. All Aetna 51-100 new business and renewing plans with December 1, 2012 and later effective dates will include a benefit feature that encourages members to use generic drugs as a first choice....
Read MorePhiladelphia Interactive HR Workshop – “Strategies from Industry Leaders in an Era of Change”
Please join Innovative at the Ultimate Software interactive HR workshop. Innovative’s own Terriann Procida will be featured speaking about how to uncover the hidden risk in your benefit package through advanced analytics and predictive modeling. Your company needs a skilled and forward-thinking HR leader more than ever before. So are...
Read MoreFive Great Whole Grains
This month we’re highlighting five whole grains that have much to offer when it comes to nutrition and flavor. The next time you’re at the supermarket or natural foods store, look for foods made with amaranth, barley, buckwheat, bulgur or quinoa and expand your whole-grain horizons. Barley The Story: Barley...
Read MoreUnited Benefit Advisors Welcomes Terriann Procida as a Board Member!
Terriann will be joining the United Benefit Advisors (UBA) Board of Directors effective January 1, 2013. As one of the nation’s largest employee benefits advisory organizations, UBA is comprised of more than 140 of the most successful and most trusted independent employee benefits advisory firms in North America and Europe. ...
Read MoreCongratulations Liz!
We are proud to announce that today Liz Silver, Innovative’s newest Account Manager, passed the third and final test to obtain her RHU designation. All that hard work paid off Liz! Congratulations on a great accomplishment!
Read MoreDid You Ever Get So Covered In Mud That…
You wondered if you would ever get clean? We did! On Saturday September 15th, teams of warriors came together at the New Jersey Motorsports Park to raise money for cancer research and to honor cancer survivors in a tribute called the Bill Bottino Mud Run. Just as cancer survivors had...
Read MoreAll That Sneezing Getting You Down?
The weather turns cooler, the leaves turn colors and pumpkins are everywhere. It’s the perfect time to enjoy the outdoors, unless you suffer from allergies. Are your eyes itchy and watery? Do you have a runny nose? Are you coughing? Does your nose itch? Do you have dark circles under...
Read MoreInnovative Speaks at MetLife Stadium!
Thank you Ultimate Software for inviting Innovative to be a part of your interactive HR workshop at MetLife Stadium yesterday in the Toyota Coaches Club! Our own Terriann Procida was asked to be a guest speaker at this fantastic event. Her presentation focused on changing the current reality of cost...
Read MoreNew Jersey Interactive HR Workshop
“Strategies from Industry Leaders in an Era of Change” Please join Innovative at the Ultimate Software interactive workshop. Innovative’s own Terriann Procida will be featured speaking about how to uncover the hidden risk in your benefit package through advanced analytics and predictive modeling. Your company needs a skilled and forward-thinking...
Read MoreMORE GUIDANCE ON “FULL-TIME” EMPLOYEES AND 90-DAY WAITING PERIOD
Starting in 2014, larger employers (generally, those with 50 or more employees) may face “shared responsibility” penalties if any of their “full-time” employees receive subsidized health coverage through an “Affordable Insurance Exchange.” At the same time, virtually all employer health plans will become subject to a 90-day limit on any...
Read MoreDo You Know What You Need To Know About Comparative Effectiveness Research Fees?
Under the Patient Protection and Affordable Care Act (PPACA), health insurers and self-funded plan sponsors will be required to pay a tax called the comparative effectiveness research fee. The proceeds are to be used to support research conducted by a Patient-Centered Outcomes Research Institute. This research will be centered on...
Read MoreIRS Issues Temporary Guidance for Identifying Full-Time Employees and Applying Waiting Periods
On Aug. 31, the IRS issued Notices 2012-58 and 2012-59, which provide safe harbors for 2014 (and perhaps beyond that date) on how to address some of the open questions on how the employer-shared responsibility penalties will apply. The notices affirm that employers that hire new employees who are reasonably...
Read MoreHealth Care Reform, Costs Likely Will Alter the Nature of Wellness
In the wake of the Supreme Court’s ruling on health care reform, the future of employer-sponsored health care insurance remains murky at best. One health trend, though, looks like it’s here to stay as more insurers, employers and workers buy into corporate wellness programs. Yet the makeup of such programs...
Read MoreEmployers Prep for New Moves under PPACA
As the 2013 enrollment time draws near, employers are preparing to jump through a few extra hoops thanks to the recently reaffirmed health care reform law. In addition to the usual notices and benefit communications that employers must prepare and distribute to their employees, the Patient Protection and Affordable Care...
Read MoreHomegrown Superfruits
Blueberries Drive anywhere in the state of Maine in the month of August and you’re likely to find a blueberry festival in progress or at least a roadside stand selling boxes of just-picked wild blueberries. Locals enjoy the little berries by the handful or in pies, muffins, jams, pancakes and...
Read MoreA Surprise for Jeannine!
When Jeannine Bandiera, Innovative Account Manager, arrived at what she thought was a client pre-renewal meeting, she was pleasantly surprised. She entered the beautifully decorated conference room and was showered with baby gifts! Jeannine would like to thank everyone at Engineering Resource Group for their thoughtfulness. Baby Bandiera will arrive...
Read MorePPACA FSA Contribution Limits
• Applies to all employers who sponsor a health flexible spending account (FSA) • Effective as of the start of the 2013 plan year May not change plan year simply to delay application of the limit • Employee salary reduction contribution may not exceed $2,500 per health FSA per year...
Read MoreLEARN WHAT YOU NEED TO KNOW ABOUT PPACA
Nearly all employers will be affected by the Patient Protection and Affordable Care Act (PPACA) — but not necessarily in the same ways. A company’s compliance requirements largely will depend on its size, method of plan funding and other factors. Do you know which provisions apply to you? As a...
Read MoreMURAL ARTS TROLLEY TOUR – A FABULOUS EVENT FOR A GREAT CAUSE!
On Wednesday July 25th, Innovative proudly sponsored the Mural Arts Program Trolley Tour hosted by the Professional Women’s Roundtable. Jane Golden, Director of the Mural Arts Program, is truly a gift to Philadelphia. Through the Mural Arts Program, Jane has used art to inspire change in communities throughout the city...
Read MoreHIGHLIGHTS OF W-2 REPORTING REQUIREMENT
• Must include the value of “employer-sponsored group health coverage” on W-2s beginning with the 2012 W-2 (to be issued in January 2013) • Except that, do not need to include this information if the employer issued fewer than 250 W-2s for the prior calendar year* o This means the...
Read MoreHIGHLIGHTS OF ADDITIONAL MEDICARE WITHHOLDING FOR HIGH EARNERS
• Effective Jan. 1, 2013 • Applies to all employers • Must withhold an additional 0.9 percent of the employee’s share for Medicare/HI (from 1.45 percent to 2.35 percent) once the employee’s wages exceed $200,000 Employer does not match this additional 0.9 percent Additional 0.9 percent is not capped Additional...
Read MoreMLR REBATE CONSIDERATIONS
Because the guidance provided by the regulatory agencies has been fairly general, employers continue to have questions about how to handle the medical loss ratio (MLR) checks. Below are answers to some common questions, based upon either the guidance issued by the agencies regarding MLRs or how similar situations have...
Read MoreCamping With Kids
Pick a Campground If you’ve never camped with children before, or you’ve never camped at all, preparing for a night outdoors may seem daunting. Your first step is to research your options: • Assemble a list of campgrounds within an hour or two of home. • Novice campers will want...
Read MoreHHS Report on MLR Provides Breakdown of Upcoming Rebates:
HHS has released a report on the first round of rebates to be provided under health care reform’s medical loss ratio (MLR) requirements. The report contains calendar year 2011 data–insurers are required to pay rebates by August 1, 2012 based on their 2011 MLR. The report provides a detailed breakdown...
Read MoreHealth Care Reform Still Stands – What Do Employers Need To Do Now?
On June 28th, the U.S. Supreme Court upheld the individual mandate and most of the Patient Protection and Affordable Care Act (PPACA). Because the individual mandate was found to be acceptable, most of the rest of the law (including the exchanges and the requirement that larger employers provide minimum coverage...
Read MoreOVERVIEW OF MEDICAL LOSS RATIO REBATES
The Affordable Care Act requires health insurers to spend a minimum percentage of their premium dollars on medical claims and quality improvement. Insurers in the large group market must achieve a medical loss ratio (MLR) of 85%, while insurers in the individual and small group markets must achieve an MLR...
Read MoreSUPREME COURT LARGELY UPHOLDS PPACA
Today, the U.S. Supreme Court upheld the individual mandate and most of the Patient Protection and Affordable Care Act (PPACA). As expected, it was a close decision — 5-4 — with Chief Justice Roberts and Justices Breyer, Ginsburg, Kagan and Sotomayor agreeing that the individual mandate is a permissible tax....
Read MoreInnovative Sponsors A Mural Arts Program Trolley Tour July 25th!
With more than 3,000 murals on display throughout the city, Philadelphia’s often referred to as the “Mural Capital of the World.” After a special visit from Mural Arts Program founder Jane Golden, we’ll hop aboard a trolley to explore the city’s incredible collection of murals with knowledgeable tour guides while...
Read MoreCompliance Alert! PREPARING FOR THE SUPREME COURT DECISION ON HEALTH CARE REFORM
The U.S. Supreme Court is expected to publish its decision on the legality of the Patient Protection and Affordable Care Act, or PPACA (also called health care reform, HCR and ACA), by the end of June. What they will decide is anyone’s guess. Here are the possibilities (in no particular...
Read MoreTHE 2012 UBA HEALTH PLAN BENCHMARKING SURVEY HAS CLOSED AND THE WINNER OF THE NEW 32 GB IPAD IS…
THE WINNERS ARE: Herr Foods, Inc. and PREIT Services, LLC!!! Due to an overwhelming response to our 2012 UBA Health Plan Benchmarking Survey we are happy to announce that we have two winners for the New 32 GB iPad! With over 17,000 plans participating, including more than 100 plans from...
Read MoreHHS Releases Guidance on Exchanges, Including Draft Exchange Blueprint and Rules for Federally Facilitated Exchanges and SHOPs
HHS has issued a flurry of guidance on Exchanges, including a draft blueprint for use by states establishing an Exchange, and an outline of the agency’s approach to implementing a federally facilitated Exchange (FFE) and federally facilitated Small Business Health Options Program (FF-SHOP) in states that do not establish a...
Read MoreFinal Regulations Address Individual Tax Credit for Coverage Purchased Through Exchange
The IRS has published final regulations addressing various aspects of the premium tax credit enacted as part of health care reform. The final regulations address a number of technical issues affecting eligibility for and calculation of the tax credit. Here are some highlights of significance for employer-sponsored plans: • Guidance...
Read MoreHHS Makes Available Calculator to Assist in Preparing Coverage Examples for SBC
As indicated in recent agency FAQs regarding the summary of benefits and coverage (SBC) requirement under health care reform, the Department of Health and Human Services (HHS) has made available a model coverage examples calculator, and related instructions and algorithm, to assist plans and insurers in preparing the required coverage...
Read MoreBorzi Announces Fee Disclosure Help for Participants
June 11, 2012 — Phyllis Borzi, assistant secretary for the Employee Benefits Security Administration (EBSA), announced tools to help participants understand fee disclosures. — In her retirement security newsletter for plan participants, Borzi said the EBSA offers consumer-focused FAQs that explain the new rules for disclosures about 401(k) services and...
Read MoreWater Precautions for the Backcountry
On day hikes, safe drinking water usually isn’t an issue. You can carry what you need. But longer, overnight adventures are another story. When planning a camping trip, it is important to anticipate your water needs. There are many approaches you can take to providing yourself and others in your...
Read MoreIRS Eases Health Care Reform Law’s $2,500 Limit for Noncalendar-Year FSAs:
The IRS on Wednesday provided regulatory relief for health care flexible spending account (FSA) participants and also said it is reconsidering its longtime use-it-or-lose-it rule for FSAs. Employer benefits lobbying groups, including the American Benefits Council (ABC) had complained that the new $2,500 annual limit set to go into effect...
Read MoreThomas Mangan Joins UBA As New CEO
The UBA Board has selected Thomas Mangan, an insurance industry leader with more than 20 years of experience in the employee benefit marketplace, to serve as chief executive officer, effective immediately. As announced at UBA’s Spring Meeting earlier this week, Thom will take over the role and duties of Bill...
Read MoreInnovative Attends the 2012 Community Access Unlimited Golf Outing
Elizabeth, NJ – May 11, 2012 – While higher is not better on golf score cards the numbers turned in by the friends, supporters and community partners of Community Access Unlimited (CAU) at the agency’s 18th Annual Golf Classic were well above par. The May 10 event at Suburban Golf...
Read MoreNew Guidance on Summary of Benefits and Coverage Adds Safe Harbors
Starting on Sept. 23, 2012, health insurers and group health plans will be required to provide the summary of benefits and coverage (SBC) and the uniform glossary to consumers. On May 11, the Department of Labor’s Employee Benefits Security Administration, together with the Departments of Health and Human Services and...
Read MoreNAHU Hosts Webinar on Exchanges
On May 10, NAHU conducted a one-hour webinar on health insurance exchanges. It was an exceptionally thorough overview of the topic, and I would encourage folks to listen/view it. The link to the Professional Development page of NAHU’s site (the webinar is the first item under the NAHU Webcasts heading):...
Read MoreMark and Nicole Attend the 8th Annual fi360 Conference in Chicago
Innovative’s Mark Sulpizio, MS Tax, AIF® and Nicole Offerman, AIF® joined approximately 600 advisors in Chicago for a three-day educational and networking event April 25th-27th. A full range of nationally recognized speakers such as Harvard Business Review editorial director and author of The Myth of the Rational Market Justin Fox...
Read MoreIs CAM Right For You?
A User’s Guide to Yoga Yoga is a mind-body practice with origins in ancient Indian philosophy. The various styles of yoga typically combine physical postures, breathing techniques and meditation or relaxation. The 2007 National Health Interview Survey found that yoga is one of the top 10 CAM practices used by...
Read MoreInnovative Exhibits at the 26th Annual Tri-State HRMA Conference
Innovative was once again thrilled to be a part of the Annual Tri-State HRMA Conference held at the Westin Hotel in Mount Laurel last Thursday. We enjoyed meeting all of the attendees while promoting our 2012 UBA Health Plan Benchmarking Survey. For anyone that started the survey there, they were...
Read MoreCOMPLIANCE ALERT!! – IRS PROPOSES METHODS FOR VALUING EMPLOYER HEALTH COVERAGE
The IRS has just issued three notices concerning key aspects of the 2010 Affordable Care Act (ACA). Notice 2012-31 proposes three different methods by which sponsors of self-funded health plans could value the coverage they provide to plan participants and their dependents. Notice 2012-32 and Notice 2012-33then solicit comments on...
Read MoreCOMPLIANCE ALERT!! – IRS PROPOSES METHODS FOR VALUING EMPLOYER HEALTH COVERAGE
The IRS has just issued three notices concerning key aspects of the 2010 Affordable Care Act (ACA). Notice 2012-31 proposes three different methods by which sponsors of self-funded health plans could value the coverage they provide to plan participants and their dependents. Notice 2012-32 and Notice 2012-33 then solicit comments on two...
Read MoreIRS ANNOUNCES 2013 AMOUNTS for HSAs and HDHPs
On April 27, the IRS issued Revenue Procedure 2012-26, announcing the 2013 inflation-adjusted dollar limitations applicable to health savings accounts (HSAs) and qualifying high-deductible health plans (HDHPs). The maximum HSA contribution for an individual with self-only coverage under an HDHP will increase to $3,250 – up from $3,100 in 2012. ...
Read MoreIRS Proposes Regulations on Fees to Fund Patient-Centered Outcomes Research
The IRS has issued proposed regulations regarding the fees imposed by health care reform on health insurers and on sponsors of self-insured health plans to support clinical effectiveness research by the new Patient-Centered Outcomes Research Institute (sometimes referred to as CER or PCOR fees). The fees apply only to policy...
Read MoreRevised Audit Guidelines
Recently, the Internal Revenue Service (IRS) published Revised Audit Guidelines for use by IRS auditors in examining group health plans for COBRA compliance. The revised Guidelines incorporate changes to account for laws that have affected COBRA since the previous guidelines were developed, such as the Health Insurance Portability and Accountability...
Read MoreHealthy Supermarket Grab-and-Go Meals
Long work hours and unfinished to-do lists often push our healthy eating habits to the back burner. But being too busy doesn’t have to be your excuse for ordering a pizza or picking up dinner at the drive-thru window. More and more, health-conscious consumers are relying on their supermarkets as...
Read MoreThe DoL Fights Employers Failing to Remit Contributions
The Labor Department’s Employee Benefits Security Administration (EBSA) has a long history of protecting the contributions employees make to their 401 (k), health care, and any other contributory plans by investigating employers who delay forwarding these contributions to the appropriate funding vehicle or who convert the contributions to other non-plan...
Read MoreState Exchange Regulations Issued
On March 12, the federal Department of Health and Human Services (HHS) released a revised version of the federal rules regarding the “Establishment of Exchanges and Qualified Health Plans and Exchange Standards for Employers.” Parts of the 644-page regulation have been issued as a final rule, meaning that they will...
Read MoreSmoking and Your Numbers
Thankfully, smoking is on the decline in the U.S., but still nearly one in five adult Americans is a smoker. Everyone knows that smoking is bad for you. And most people cite lung cancer as the primary reason for quitting. But that isn’t the only reason to quit: •Smoking raises...
Read MoreKnow Your Numbers – Four Steps
You’re up-to-date on your health screenings. You and your doctor have gone over your numbers together. She points out that your BMI, cholesterol and blood pressure have inched up just a bit over the past couple of years and advises you to “watch what you eat” and to “get more...
Read MoreAgencies Issue Guidance on Waiting Periods
Under the ACA, effective for plan years beginning on or after January 1, 2014, a group health plan may not have a waiting period that exceeds 90 days. The ACA’s statutory language raised many questions regarding how this 90-day limit on waiting periods should be measured. Notice 2012-17 continues to...
Read MoreThe Innovative Award Goes To…
Innovative would like to congratulate UBA partner firm principal, Paul Bogumill of Mountain West Benefits in Helena, Montana, for receiving the Innovative Award at the annual Pharmacy Benefit Management Institute conference in Phoenix, Arizona. Paul was the brainchild behind the development of a new, innovative pharmacy benefit called URx. At...
Read MoreAgencies Issue Guidance on Employer Mandate
Employer Shared Responsibility A key element of the ACA is the employer “shared responsibility” provision. This provision, currently scheduled to take effect in 2014, would assess a penalty against certain “applicable large employers” (those with 50 or more full-time employees) that either fail to offer “minimum essential coverage” to their...
Read MoreAGENCIES ISSUE GUIDANCE ON AUTOMATIC ENROLLMENT
The ACA provision on automatic enrollment requires certain large employers (those with more than 200 full-time employees) to automatically enroll new full-time employees in one of the employer’s health benefit plans (subject to any legally permissible waiting period), and to continue the enrollment of current employees in a health benefit...
Read More2012 UBA HEALTH PLAN BENCHMARKING IS NOW OPEN!!!
Participate in the 2012 Survey and Receive a Detailed Benchmarking Analysis The 2011 survey gathered results from 16,421 health plans from 10,744 employers — making it the largest benchmarking survey of employer-sponsored health care plans in the country. The results provided critical national and regional benchmarks that enabled companies to...
Read MoreThe Innovative Way!
Great job by Innovative’s Jeannine Bandiera, who found a way to make a member’s medication affordable! Recently one of our members was made aware of a tier change for the medication that she needs to treat her condition. The insurance carrier moved the medication to the Specialty Drug list from...
Read MoreMilliman Study Highlights the Impact of Medical Loss Ratio Rules on HSAs
A new report by Milliman Inc. says that high-deductible health plans, including those with health savings accounts (HSAs), will likely be more adversely impacted by the medical loss ratio requirements under PPACA than other types of comprehensive medical plans. Consumers who rely on HSA-qualified plans to finance their health care...
Read MoreHHS Releases Guidance Related to Annual Dollar Limit Waivers
On Feb. 13, 2012, the Department of Health and Human Services (HHS) stated a health insurance issuer that has received a waiver of the annual dollar limit requirements pursuant to Section 2711 of the Public Health Service Act for a group health insurance product can sell that product to a...
Read MoreAgencies Finalize Guidance On Summary Of Benefits And Coverage
As explained in our August 2011 article, the health care reforms enacted in March of 2010 will require employer health plans to provide a uniform “summary of benefits and coverage” (SBC) to all plan participants and beneficiaries. The agencies charged with implementing this requirement have now finalized the regulations they...
Read MoreHealthy Skin, Healthy Living
Glowing, spotless, wrinkle-free skin is much valued in our society. We’re willing to spend a lot for that look. It’s estimated that the skin care industry in the U.S. is worth about $43 billion per year. But healthy skin starts from the inside, not just from creams and lotions applied...
Read MoreDOL, HHS and Treasury Issue Technical Release on Automatic Enrollment, Waiting Periods and Employer Shared Responsibility
The Employee Benefits Security Administration (EBSA) has issued Technical Release 2012-01, which provides information on questions from employers and other stakeholders regarding the provisions of the Patient Protection and Affordable Care Act (PPACA) governing automatic enrollment, employer shared responsibility, and the 90-day limitation on waiting periods. These provisions are scheduled...
Read MoreAgencies Release PPACA Final Rule, Guidance and Templates for Summary of Benefits and Coverage (SBC) and Uniform Glossary of Terms
The Departments of Labor, Treasury and Health and Human Services have released final regulations under the Patient Protection and Affordable Care Act (PPACA) that require health insurers and group health plans to provide concise and comprehensible information about health plan benefits and coverage to those with private health coverage. Under...
Read MoreInnovative’s Mark Sulpizio Goes To The Harvard Club
On Wednesday, February 8, 2012 our own Mark Sulpizio attended Federated Investors’ Retirement Security Symposium at The Harvard Club of New York City. This special event was by invitation only and featured The Honorable Bradford P. Campbell as the Key Note Speaker. Mr. Campbell formerly served as the Assistant Secretary...
Read MoreDOL Finalizes, Delays 401(k) Fee Disclosure Rules
After months of delay, the Department of Labor (DOL) has just released final regulations under Section 408(b)(2) of ERISA, requiring retirement plan service providers to disclose information about their services and fees to plan sponsors. In doing so, the DOL delayed the effective date of those rules and made minor...
Read More2012 Fiscal Year Plans Must Adhere to FSA $2,500 Limit
Though not the norm, some Cafeteria Plans (Section 125 plans) are not calendar year plans but instead are fiscal year plans (e.g. February 1-January 31). Be careful if this applies to you because if your fiscal year plans include Health Care Spending Accounts (HCSA), then as the plan sponsor, you...
Read MoreIRS Releases 2011 Form 8941 and Instructions for Claiming
The IRS has released the 2011 version of Form 8941, which is used by eligible small employers to calculate their health care tax credit. Once calculated, the tax credit is claimed as a general business credit on Form 3800 (or by tax-exempt small employers as a refundable credit on Form...
Read MoreHHS Secretary Announces One-Year Delay for Nonprofits with Religious Beliefs in Complying with No-Cost Women’s Preventive Services
After receiving comments on the interim final rule requiring most health insurance plans to cover preventive services for women including recommended contraceptive services without copays, coinsurance or deductibles, Health and Human Services (HHS) Secretary Kathleen Sebelius announced that nonprofit employers who, based on religious beliefs, do not currently provide contraceptive...
Read MoreMore IRS Guidance On W-2 Reporting of Health Coverage
_ Overview of Reporting Requirement _ Before addressing the recent guidance, it is worth noting some key points that have not changed. For instance, this reporting requirement remains optional for 2011, but then required for 2012. Also preserved is a postponement of this requirement for “small” employers. Any employer that...
Read MoreDo You Like To Eat Out?
Our own Terriann Procida is Chairperson for this year’s Samaritan Healthcare & Hospice Gala taking place February 25th in Mt. Laurel, NJ. As part of the fundraiser we are selling raffle tickets for $5 to win 12, $200 Gift Certificates to the following restaurants: Amada, Brio, Caffe Aldo Lamberti, Cafe Madison,...
Read MoreIRS Issues Additional Guidance on Form W-2 Health Care
The U.S. Internal Revenue Service (IRS) has issued Notice 2012-9 to provide additional guidance on the informational reporting to employees of the cost of their employer-sponsored group health plan coverage on Form W-2. The IRS requested public comments on the W-2 reporting requirement in Notice 2011-28. Notice 2012-9 responds to...
Read MoreSoup’s On!
Several studies show that soup eaters end up weighing less than those who don’t eat much soup, according to Penn State nutrition professor Barbara Rolls, co-author of “Volumetrics: Feel Full on Fewer Calories.” “Incorporating soups into a weight-management plan can really help save calories,” she notes. She also likes it...
Read MoreFinal Rule for CO-OPs – Highlights
On Dec. 8, the Centers for Medicare and Medicaid Services (CMS) released the Final Rule produced by the Department of Health and Human Services (HHS) to establish the Consumer Operated and Oriented Plan (CO-OP) Program under Section 1322 of the Patient Protection and Affordable Care Act (PPACA). The following are...
Read MoreEssential Health Benefits: HHS Informational Bulletin
On Dec. 16, the Department of Health and Human Services (HHS) issued a bulletin outlining the approach (and proposed policies) that HHS intends to pursue in rulemaking to define essential health benefits. The bulletin can be found at http://www.healthcare.gov/news/factsheets/2011/12/essential-health-benefits12162011a.html.
Read MoreEarly Retiree Reinsurance Program Wrapping Up
The Early Retiree Reinsurance Program will cease to be operational in short order. The $5 billion program was created in July of 2010 to help offset employer costs associated with providing health coverage benefits to early retirees and their eligible spouses, surviving spouses, and dependents. From the get-go, experts predicted...
Read MoreHHS Releases FAQs on Implementation of Exchanges, Including Issues Raised by Federally Facilitated Exchanges
On Nov. 29, HHS released 13 Q&As addressing implementation issues for state and federally facilitated Exchanges. The Q&As cover a range of topics including funding responsibility and resources, information exchanges through federally managed data “hubs,” and shared eligibility verification services. Among them are Q&As focused on issues raised by federally...
Read MoreW-2 Reporting Requirements
Requires all employers (including government entities) to include the aggregate cost (whether paid by the employer or the employee) of employer-sponsored health benefits on the employees’ annual Form W-2. The specific value attributable to each benefit is not required. If an employee receives health insurance coverage under multiple plans, the...
Read MoreCMS Releases PPACA Medical Loss Ratio Requirements Including Group Health Plan Rebate Provisions
On Dec. 2, the Centers for Medicare & Medicaid Services (CMS) issued a final regulation that will ensure health insurance companies spend at least 80 percent of consumers’ health insurance premiums on medical care, not income, overhead and marketing. Insurance companies that fail to meet the new standard are required...
Read MoreBefore You Go: Healthy Travel Tips
Need a Flu Shot? With all that’s going on at this time of year, getting vaccinated against seasonal flu may be the last thing on your mind. But you don’t want to come down with the flu when you’re away from home. And you certainly don’t want to spread the...
Read MoreFiduciary Luncheons A Success Again!
Innovative would like to thank all of our guests that attended the Fiduciary Luncheons that we hosted last week in Princeton, Parsippany and Philadelphia. Innovative’s own Mark Sulpizio, Accredited Investment Fiduciary®, discussed the impact of the new 408(b)(2) and 404(a) fee disclosure regulations. Mark also touched on what fiduciary best practices...
Read MoreEmployer Health Care Reform Law Communication Mandate Delayed
Employers have more time to comply with rules dictated by the health care reform law that will require them to revamp how they communicate and explain their health care plans. In a notice published Nov. 17, the Department of Labor (DOL) said the reporting requirements would not go into effect...
Read MoreNJ Posting and Notification Requirements for Employers
The NJ Department of Labor and Workplace Development issued a new regulation concerning employer obligations and their record keeping. For employees hired after November 7, 2011 a written copy of the form notification of these regulations must be distributed at the time of hiring. For existing employees a document must...
Read MoreHealth Law May Undermine Marriage
The health reform law could undermine marriage because once people tie the knot, they may no longer be eligible for tax incentives for insurance. The law links the tax credit to household income, so two people whose combined income goes above a certain level will not be able to get...
Read MoreYear-End Notices for Retirement Plans
There are a series of notices regarding retirement plans that must be provided to participants as the end of 2011 approaches. Included in these notices are the following: 1) If a plan sponsor makes “safe harbor” 401(k) contributions, the plan sponsor must provide the participants with a safe harbor notice...
Read MoreCancer Prevention on Your Plate – Quick Takes For Cancer Prevention
Screening tests are one important element of cancer prevention. Healthy lifestyle choices are another. Your cancer prevention strategy should include these positive choices: Don’t neglect cancer screenings: Early detection saves lives. Avoid tobacco: Cutting out tobacco will immediately reduce your risk for cancer of the lung, throat, bladder, kidney, pancreas...
Read MoreHHS Releases Recommendation to Halt CLASS Act
The Obama administration on Friday pulled the plug on a voluntary long-term care program that was part of the health care reform law. “We have not identified a way to make CLASS work at this time,” Health and Human Services Secretary Kathleen Sebelius said. Because the program was voluntary, critics...
Read MorePosting of Employee Rights Notice Extended; Now Required on Jan. 31
The National Labor Relations Board (NLRB) has postponed the implementation date for its new notice-posting rule by more than two months in order to allow for enhanced education and outreach to employers, particularly those who operate small and midsize businesses. The new effective date of the rule is Jan. 31,...
Read MoreNew Site Shows Health Insurance Rate Hikes
Beginning now, consumers across the country can click their state on a federal webpage to see if a health insurer has raised its rates, as well as the company’s reason for doing so. The new site will also include a section where consumers can comment about rate increases. Beginning Sept....
Read MoreIOM Issues Report for HHS Recommending Criteria and Methods
A new Institute of Medicine (IOM) report provides the U.S. Department of Health and Human Services (HHS) with a set of criteria and methods to develop a package of essential health benefits that will cover many health care needs, promote medically effective services and be affordable to purchasers. Certain insurance...
Read MoreJobs Bill Would Cap Employer Exclusion and HRA/HSA Deductions
The release of President Barack Obama’s deficit reduction plan comes just a week after the President submitted to Congress the actual text of his proposed jobs legislation. The bill, S.1549 , would change the tax treatment of employer-sponsored health insurance. Section 401 of the bill limits the value of all...
Read MoreCMS Proposes Updates to Medicare Advantage and Part D Coverage
The Centers for Medicare and Medicaid (CMS) has issued 298 pages of proposed revisions to the Medicare Advantage program and prescription drug benefit program (Part D) that would implement new benefits under the Patient Protection and Affordable Care Act (PPACA) and increase patient protections. The proposals would codify provisions providing...
Read MoreU.S. Plan Would Boost Access to Lab Results
The Obama administration proposed a new rule that would allow patients to have direct access to electronic medical records, including lab results without waiting to hear them from a doctor. At present, patients can only obtain lab results if their physicians provide authorization, or if they reside in a few...
Read MoreCMS Issues Changes to Claims Submissions for Early Retiree Reinsurance Program
The Centers for Medicare and Medicaid Services (CMS) has announced several changes to improve and streamline the process of submitting claims data for Early Retirement Reinsurance Program (ERRP) reimbursement requests. On Monday, Oct. 3, 2011, CMS will begin providing specific, claim line-level feedback to sponsors who submit claim lists through...
Read MoreCMS Issues Changes to Claims Submissions for Early Retiree Reinsurance Program
The Centers for Medicare and Medicaid Services (CMS) has announced several changes to improve and streamline the process of submitting claims data for Early Retirement Reinsurance Program (ERRP) reimbursement requests. On Monday, Oct. 3, 2011, CMS will begin providing specific, claim line-level feedback to sponsors who submit claim lists through...
Read MoreInnovative Speaks in Dallas!
At the Fall 2011 United Benefit Advisors (UBA) Meeting in Dallas, Innovative’s own Mark Sulpizio and Terriann Procida spoke to over 300 members from across the country. Recognized as experts in the retirement plan industry, they discussed the added scrutiny and fiduciary responsibility for retirement plan sponsors, in light of...
Read MoreInnovative Congratulates Jim Edwards!
Innovative would like to congratulate UBA partner firm president, Jim Edwards of Mountain West Benefits in Helena, Montana, for having been chosen by Employee Benefit Adviser magazine as 2011 Health Plan Adviser of the Year. Mountain West Benefits proudly represented UBA firms with this honor and demonstrated the forward-thinking cost...
Read MoreTibble v. Edison International, A Lesson in Revenue Sharing
When you sponsor a retirement plan you, or someone you appoint, are responsible for making many important decisions associated with the plan such as investment options and service providers. Informed decision making is reliant upon understanding and evaluating the costs associated with the plan. One of the costs inherent in...
Read MoreProposed Regulations to Make Health Insurance Shopping Easier for Consumers
As part of the Patient Protection and Affordable Care Act (PPACA) the Department of Labor and the Department of Health and Human Services has proposed some new regulations centered around clarifying health plan benefits and coverage for consumers. Many consumers feel overwhelmed when trying to decide which plan to take...
Read MoreHealth Law’s Premium Rate-Review Provision
Under a health reform law provision that goes into effect Sept. 1, states and the federal government will scrutinize health insurance company’s proposals for rate increases on individual and small-employer plans. Insurers will be required to submit a seven-page document, justifying the increase to the Department of Health and Human...
Read MoreEBSA FAQ Clarifies End of COBRA ARRA Subsidy
The Department of Labor’s Employee Benefits Security Administration (EBSA) updated its web page to clarify the end of the COBRA ARRA subsidy. FAQ Q1 states that some individuals are eligible to receive the COBRA premium reduction subsidy beyond Aug. 31, 2011. Individuals who qualified on or before May 31, 2010...
Read MoreCBO Predicts Delay In Start Of CLASS Program
The Congressional Budget Office (CBO) anticipates a one-year delay in implementation of the Community Living Assistance Services and Supports (CLASS) Act included in last year’s health reform bill. In its latest periodic update to Congress on the federal budget, the CBO notes that based on the pace of implementation of...
Read MoreNew Rule Requires Non-Union Employers To Notify Employees Of Their Right To Unionize
The National Labor Relations Board (NLRB) has just issued a final rule obligating the vast majority of private sector employers to notify employees of their rights under the National Labor Relations Act (NLRA). The purpose of the notice is to inform employees of their rights to organize, form, join or...
Read MoreConsumer Driven Health Plan Growth Slows; Costs Surpass HMOs
Cinnaminson, NJ, August 29, 2011 -Consumer Driven Health Plans (CDHPs) in the U.S. experienced continued growth this year – albeit at a slower rate than in 2009 and 2010 – according to preliminary results released by United Benefit Advisors (UBA) from its 2011 UBA Health Plan Survey, the nation’s largest...
Read MoreNew Exchange Subsidy, Medicaid Expansion and Premium Tax Credit Regulations Released
The Obama administration put out three proposed rules (comprising 409 pages) on Friday that will be critical to the establishment of health insurance exchanges. Two of the rules came from the Department of Health and Human Services (HHS): The first rule (139 pages) outlines exchange eligibility and employer standards. The...
Read MoreFederal Appeals Court Rules Against PPACA’s Individual Mandate
Since the enactment in 2010 of the Affordable Care Act’s requirement that all Americans must carry health insurance or face a tax penalty there has been controversy over the constitutionality of the mandate. When the White House passed the law the administration argued that the legislative branch has the ability...
Read MoreAffordable Care Act Ensures Women Receive Preventive Services at No Additional Cost
Historic new guidelines that will ensure women receive preventive health services at no additional cost were announced today by the U.S. Department of Health and Human Services (HHS). Developed by the independent Institute of Medicine, the new guidelines require new health insurance plans to cover women’s preventive services such as...
Read MoreEBSA Extends 408(b)(2) to April 2012
The Employee Benefits Security Administration, an arm of the U.S. Department of Labor, has extended the effective date for the interim final fiduciary-level fee disclosure rule, 408(b)(2), from July 16, 2011 to April 1, 2012. Initially proposed in the summer of 2010, the Department ruled to enhance the required fee...
Read More$10 Million In Funding Available For Workplace Health Programs
In addition to the President’s Childhood Obesity Task Force, the First Lady’s Let’s Move initiative, and the National Prevention Council, which was formed to design and implement a National Prevention and Health Promotion Strategy, the government has now embarked upon another area of wellness, this time aimed at supporting workplace...
Read MoreVoucher Provision Repealed
After much negotiation and the threat of a government shutdown the budget was passed last week. This is good news for employers as members of Congress agreed to have the Voucher Provision taken out of the Patient Protection and Affordable Care Act (PPACA) in an effort to reduce the budget. ...
Read MoreHHS Provides Illustrative Information Regarding Benchmarks for Essential Health Benefits
The Department of Health and Human Services (HHS) provided illustrative information to complement its Dec. 16, 2011, bulletin on essential health benefits (EHB) under the Patient Protection and Affordable Care Act. The information provides the names of the three largest products in the small group market in each state ranked...
Read MoreSamaritan Hospice Announces Gala
As posted on Patch.com By Patch Staff Email the author January 7, 2011 Samaritan Hospice will hold its 30th annual gala Feb. 26 at The Westin Mt. Laurel, CEO Mary Ann Boccolini announced. “I am pleased that Terriann Procida of Moorestown, President of Innovative Benefit Planning LLC in Cinnaminson agreed...
Read MoreMedicare Secondary Reporting Requirements for HRAs
Beginning 10/1/10, HRA plans are required to report on a quarterly basis all covered HRA participants and dependents that meet specific criteria. The purpose of reporting is to enable CMS to correctly pay for health insurance benefits of Medicare beneficiaries by determining primary vs. secondary payer responsibility. The employee/dependent data...
Read MoreModel Notices on PPACA Grievance and Appeal Rules
The Department of Labor this week published its model notices under the PPACA Claims and Appeals Regulation, providing model notices that can be used in connection with adverse benefit determinations, appeals of adverse benefit determinations, and a final external review decision. DOL also published Technical Release 2010-1, which provides an...
Read MoreNotice Published in Federal Register on Lifetime Income Options for Retirement Plans
The Agencies published in the Federal Register a request for information (RFI) regarding whether, and, if so, how, by regulation or otherwise, it would be appropriate for them to enhance the retirement security of participants in employer-sponsored retirement plans and in individual retirement arrangements (IRAs) by facilitating access to, and...
Read MoreThe Occupational Training Center of Camden County
We recently partnered with the Occupational Training Center in Berlin NJ to help us put together some of our promotional items. We have had great feedback and success on the work they have done for us. The OTC is a great partner to hiring high paid temporary services or running...
Read MorePreventive Care Regulation Released
On Wednesday, the Departments of Health and Human Services, Labor and Treasury released an interim final regulation outlining the details of the preventive care coverage requirement for health plans established by the Patient Protection and Affordable Care Act (PPACA). PPACA requires that all plans provide first-dollar coverage of specific preventive...
Read MorePA Mini-Cobra Extended
On July 9th, Governor Rendell signed House Bill 1251 that included a change to Pennsylvania Mini-COBRA to allow for coverage beyond 9 months if a covered individual is also receiving a federal premium subsidy. This means that individuals who are eligible for the premium subsidy under the American Recovery and...
Read MoreNew Break Time Requirement for Nursing Mothers
The United States Department of Labor’s Wage and Hour Division recently released a Fact Sheet providing guidance on the new break time requirement for nursing mothers. This new requirement took effect when Section 7 of the Fair Labor Standards Act (“FLSA”) was amended by the Patient Protection and Affordable Care...
Read MoreInterim Final Rule on Internal Claims and Appeals and External Review Processes Released
New Regulations Give Patients Right To Appeal Health Plan Decisions; New Grants Program Strengthens State and Territory Consumer Assistance Programs The Obama Administration is announcing both new regulations to empower consumers to appeal decisions made by their health plans or insurance companies and the availability of resources that will be...
Read MoreRegulations Issued on Lifetime and Annual Limits
Close on the heels of their regulations concerning grandfathered plans, the Departments of Labor, Health and Human Services (HHS), and Treasury have now released interim final regulations relating to preexisting condition exclusions, lifetime and annual limits, rescissions, and other patient protections under the Affordable Care Act (the “Act”). Lifetime Limits...
Read MoreIBP sponsors 401(k) Educational Luncheon
Mark Sulpizio, a founding partner at IBP, was the presenter at a qualified plan educational luncheon held at Union Trust Steakhouse in Philadelphia on Thursday, July 22 2010. At the luncheon, Mark reviewed the recently released 408(b)(2) “interim final regulations” from the Department of Labor and how the new rules...
Read MoreFiduciary Update – The SEC and Target Date Branding
As discussed at our recent fiduciary luncheon events, the regulatory agencies are continuing to look at target date funds. Last week, the commissioners at the SEC approved new regulations regarding the marketing of target date funds. The agency wants to require the use of a visual aid illustrating the funds...
Read More5500 Efast Filing
As you may already be aware, new regulations were recently passed requiring all sponsors of qualified plans to file their Form 5500 and accompanying schedules electronically beginning January 1, 2010. Hard copies will no longer be accepted, rather will need to be submitted via the Department of Labor’s EFAST2 electronic...
Read MoreInnovative Sponsors 401(k)/403(b) Fiduciary Luncheon
Mark Sulpizio, a founding partner at IBP, presented a workshop on the added fiduciary responsibilities plan sponsors will face due to the upcoming Department of Labor 408(B)(2) regulations at Ruth’s Chris Steak House in Princeton, NJ. The program reviewed what plan sponsors should be doing to prepare for the regulations...
Read MoreUS Dept. of Health & Human Services, Labor & Treasury Issue Regulation on “Grandfathered” Health Plans Under the Affordable Care Act
While the Affordable Care Act requires all health plans to provide new mandated benefits under the law, plans that existed on March 23, 2010 are exempt from some new requirements. The U.S. Departments of Health and Human Services, Labor, and Treasury issued new regulations on “Grandfathered” health plans under the Affordable...
Read MoreInnovative Presents on Healthcare Reform
Terriann Procida, one of our founding partners, had the privilege of delivering an informative talk about Healthcare Reform on Wednesday, June 9th in Philadelphia. She covered topics such as The Patient and Affordable Care Act as well as the Health Care and Education Reconciliation Act of 2010, both of which have...
Read MoreHopeWorks Charity Golf Classic
Innovative Benefit Planning attended the annual HopeWorks Charity Golf Classic on Monday, June 7th at the Laurel Creek Country Club in Moorestown, NJ. HopeWorks seeks to achieve D.R.E.A.M.S. (Dynamic Realizable Efforts to Attain and Maintain Success) for inner-city Camden, NJ youth by expanding the learning opportunities available to them. Innovative, which was one of...
Read MoreMarch 2010 Retirement Plan Update Part 1
It has been a busy year in Washington with stimulus, cap and trade and health care dominating the headlines. Behind the scenes, it has also been a busy year for proposals that will affect how employers manage their retirement plans. Currently, there is pending legislation in Washington regarding participant level investment advice and the way advisors are compensated...
Read MoreNew Website Launched!
Innovative is pleased to announce the launch of our new website. The site will make it easier for clients to register for events, locate previous compliance alerts and most importantly provide us with feedback for our services. So please stop by the site and let us know what you think!...
Read MoreCategories
Archive










